Ventricular Tachycardia: Difference between revisions
mNo edit summary |
mNo edit summary |
||
| (6 intermediate revisions by the same user not shown) | |||
| Line 17: | Line 17: | ||
Ventricular tachycardia is defined as a sequence of three or more ventricular beats. The frequency must by higher than 100 bpm, mostly it is 110-250 bpm. | Ventricular tachycardia is defined as a sequence of three or more ventricular beats. The frequency must by higher than 100 bpm, mostly it is 110-250 bpm. | ||
Ventricular tachycardias often origin around old scar tissue in the heart, e.g. after myocardial infarction. Also electrolyte disturbances and ischemia can cause ventricular tachycardias. The cardiac output is often strongly reduced during VT resulting in hypotension and loss of conciousness. VT is a medical emergency as it can deteriorate into [[#Ventricular fibrillation|Ventricular fibrillation]] and thus mechanical cardiac arrest. | Ventricular tachycardias often origin around old scar tissue in the heart, e.g. after myocardial infarction. Also electrolyte disturbances and ischemia can cause ventricular tachycardias. The cardiac output is often strongly reduced during VT resulting in hypotension and loss of conciousness. VT is a medical emergency as it can deteriorate into [[#Ventricular fibrillation|Ventricular fibrillation]] and thus mechanical cardiac arrest. Although ventricular tachycardia is often associated with cardiac disease, short non-sustained VTs during exercise in otherwise healthy individuals, are not necesarrily associated with a worse prognosis <cite>NSVT</cite>. | ||
Ventricular tachycardia can be catechorized as follows: | Ventricular tachycardia can be catechorized as follows: | ||
| Line 25: | Line 25: | ||
*'''Polymorphic VT''': the ventricular beats have a changing configuration. The RR interval is 180-600 ms (comparable to a heart rate of 100-333 bpm). | *'''Polymorphic VT''': the ventricular beats have a changing configuration. The RR interval is 180-600 ms (comparable to a heart rate of 100-333 bpm). | ||
*'''Biphasic VT''': a ventricular tachycardia with a QRS complex that alternates from beat to beat. Associated with [[Miscellaneous#Digoxin|digoxin intoxication]] and [[lqts|long QT syndrome]]. | *'''Biphasic VT''': a ventricular tachycardia with a QRS complex that alternates from beat to beat. Associated with [[Miscellaneous#Digoxin|digoxin intoxication]] and [[lqts|long QT syndrome]]. | ||
Ventricular tachycardia can be difficult to diagnose when confronted with a wide complex tachycardia. A seperate chapter deals with [[Approach_to_the_Wide_Complex_Tachycardia|ECG algorithms to analyze wide complex tachycardias]]. | |||
==Localisation of the origin of a ventricular tachycardia== | |||
The localisation of the origin (or exit site) of a ventricular tachycardia can be helpful in understanding the cause of the VT and is very helpful when planning an ablation procedure to treat a ventricular tachycardia. [[Localisation of the origin of a ventricular tachycardia]] is discussed in a seperate chapter. | |||
==Examples== | ==Examples== | ||
<gallery > | <gallery > | ||
| Line 32: | Line 39: | ||
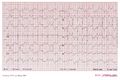
Image:12lead_vt4.jpg|Ventricular tachycardia of 145 bpm with a [[RBBB|right bundle branch block]] pattern and left [[heart axis]]. | Image:12lead_vt4.jpg|Ventricular tachycardia of 145 bpm with a [[RBBB|right bundle branch block]] pattern and left [[heart axis]]. | ||
Image:nsvt.png|A non sustained VT of five beats duration | Image:nsvt.png|A non sustained VT of five beats duration | ||
Image | Image:ECG000006.jpg|An example of idiopathic ventricular tachycardia (Belhassen VT) | ||
File:DVA2161.jpg|A biphasic VT in a patient with long QT syndrome | File:DVA2161.jpg|A biphasic VT in a patient with long QT syndrome | ||
</gallery> | </gallery> | ||
==References== | |||
<biblio> | |||
#segal pmid=17338765 | |||
#NSVT pmid=23747767 | |||
</biblio> | |||
Latest revision as of 20:33, 25 August 2013
| This is part of: Ventricular Arrhythmias |
Ventricular tachycardia is defined as a sequence of three or more ventricular beats. The frequency must by higher than 100 bpm, mostly it is 110-250 bpm.
Ventricular tachycardias often origin around old scar tissue in the heart, e.g. after myocardial infarction. Also electrolyte disturbances and ischemia can cause ventricular tachycardias. The cardiac output is often strongly reduced during VT resulting in hypotension and loss of conciousness. VT is a medical emergency as it can deteriorate into Ventricular fibrillation and thus mechanical cardiac arrest. Although ventricular tachycardia is often associated with cardiac disease, short non-sustained VTs during exercise in otherwise healthy individuals, are not necesarrily associated with a worse prognosis NSVT.
Ventricular tachycardia can be catechorized as follows:
- Non-sustained VT: three or more ventricular beats with a maximal duration of 30 seconds.
- Sustained VT: a VT of more than 30 seconds duration (or less if treated by electrocardioversion within 30 seconds).
- Monomorphic VT: all ventricular beats have the same configuration.
- Polymorphic VT: the ventricular beats have a changing configuration. The RR interval is 180-600 ms (comparable to a heart rate of 100-333 bpm).
- Biphasic VT: a ventricular tachycardia with a QRS complex that alternates from beat to beat. Associated with digoxin intoxication and long QT syndrome.
Ventricular tachycardia can be difficult to diagnose when confronted with a wide complex tachycardia. A seperate chapter deals with ECG algorithms to analyze wide complex tachycardias.
Localisation of the origin of a ventricular tachycardia
The localisation of the origin (or exit site) of a ventricular tachycardia can be helpful in understanding the cause of the VT and is very helpful when planning an ablation procedure to treat a ventricular tachycardia. Localisation of the origin of a ventricular tachycardia is discussed in a seperate chapter.
Examples
-
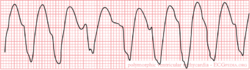
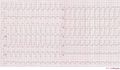
Ventricular tachycardia of 140 bpm with a left bundle branch block pattern and left heart axis.
-
Ventricular tachycardia of 250 bpm with a right bundle branch block pattern and right heart axis.
-
Ventricular tachycardia of 150 bpm with a right bundle branch block pattern and right heart axis. Mind the 5th and 6th complex from the right side. These are fusion complexes. Furthermore this ECG shows baseline drift, which is a technical artefact
-
Ventricular tachycardia of 145 bpm with a right bundle branch block pattern and left heart axis.
-
A non sustained VT of five beats duration
-
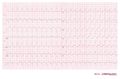
An example of idiopathic ventricular tachycardia (Belhassen VT)
-
A biphasic VT in a patient with long QT syndrome
References
<biblio>
- segal pmid=17338765
- NSVT pmid=23747767
</biblio>