Supraventricular Rhythms: Difference between revisions
Jump to navigation
Jump to search
m (New page: ==Narrow complex tachycardias== ===Atrial flutter=== {{Arrhythmias| | name = Atrial flutter | locatieImage = 250px | atrial_frequency = 250-350 bpm | ...) |
mNo edit summary |
||
| (55 intermediate revisions by 10 users not shown) | |||
| Line 1: | Line 1: | ||
{{authors| | |||
|mainauthor= [[user:Drj|J.S.S.G. de Jong]] | |||
|moderator= [[user:Drj|J.S.S.G. de jong]] | |||
{{ | |supervisor= | ||
| | |||
| | |||
| | |||
| | |||
| | |||
}} | }} | ||
===Supraventricular tachycardias=== | |||
{| class="wikitable" border="1" width="610px" | |||
|- | |||
| [[Image:atrial_ventricular.png|300px]] | |||
| [[image:SVT_overview.svg|300px]] | |||
| [[Image:Svt_algorythm_en.png|300px]] | |||
|- | |||
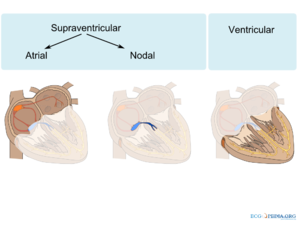
!Arrhythmias are categorized into supraventricular and ventricular depending on their origin (below the bifurcation of the His bundle is ventricular) | |||
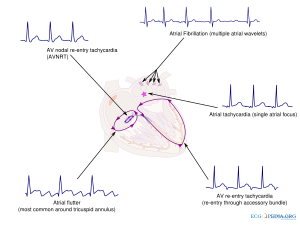
!An overview of pathological supraventricular arrhythmias and their origin | |||
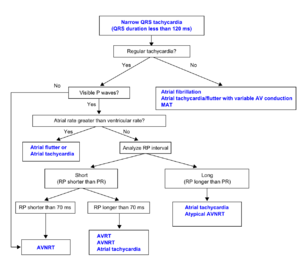
!Algorithm to diagnose SVTs<cite>ACC</cite> | |||
|} | |||
{| class="wikitable" font-size="90%" | |||
|- style="text-align:center;background-color:#6EB4EB;" | |||
|+'''An overview of supraventricular tachycardias''' | |||
|- | |||
! | |||
!Example (lead II) | |||
!Regularity | |||
!Atrial frequency | |||
!Ventricular frequency | |||
!Origin (SVT/VT) | |||
!P-wave | |||
![[Effect of adenosine]] | |||
|- | |||
| colspan="8" style="text-align:left;background-color:#cfefcf;" | '''Narrow complex (QRS<0.12)''' | |||
|- | |||
! [[Sinustachycardia]] | |||
| [[Image:sinustachy_small.svg|200px|Sinustachycardia - a normal p wave precedes every QRS complex]] | |||
| regular | |||
| 100-180 bpm | |||
| 100-180 bpm | |||
| sinusnode (SVT) | |||
| precedes every QRS complex | |||
| gradual slowing | |||
|- | |||
! [[Atrial Fibrillation]] | |||
| [[Image:afib_small.svg|200px|Atrial fibrillation - irregular rate, no p waves]] | |||
| grossly irregular | |||
| 400-600 bpm | |||
| 75-175 bpm | |||
| atria (SVT) | |||
| absent | |||
| slows down rate; irregularity remains | |||
|- | |||
! [[Atrial Flutter]] | |||
| [[Image:aflutt_small.svg|200px|Atrial flutter - sawtooth in lead II with 2:1 block]] | |||
| regular (sometimes alternating block) | |||
| 250-350 bpm | |||
| 75-150 bpm (3:1 or 2:1 block is most common) | |||
| atria (SVT) | |||
| negative sawtooth in lead II | |||
| temporary reduced conduction (e.g. 4:1) | |||
|- | |||
! [[AVNRT]] | |||
| [[Image:avnrt_small.svg|200px|ANVRT - rSR' in lead V1]] | |||
| regular | |||
| 180-250 bpm | |||
| 180-250 bpm | |||
| AV-node (SVT) | |||
| in QRS complex (R') | |||
| stops | |||
|- | |||
! [[Atrial Tachycardia]] | |||
| [[Image:atrialtachy_small.svg|200px|Atrial tachycardia - like sinustachycardia but the p wave has a different morphology]] | |||
| regular | |||
| 120-250 bpm | |||
| 75-200 bpm | |||
| atria | |||
| precedes QRS, p wave differs from sinus-p | |||
| temporary AV-block | |||
|- | |||
! [[AVRT|Atrio-Ventricular Reentry Tachycardia (AVRT)- orthodromic]] | |||
| [[Image:avrt_small.svg|200px|AVRT - inverted p wave behind every QRS complex]] | |||
| regular | |||
| 150-250 bpm | |||
| 150-250 bpm | |||
| circle: av-node - ventricles - bypass - atria | |||
| RP < PR | |||
| stops | |||
|- | |||
! [[AVJT|AV junctional tachycardia]] | |||
| [[Image:avnodal_small.svg|200px|AV junctional tachycardia - no or inverted p-waves within QRS complex]] | |||
| regular | |||
| 60-100 bpm | |||
| 70-130 bpm | |||
| AV node | |||
| RP < PR | |||
| reduces rate | |||
|- | |||
| colspan="8" style="text-align:left;background-color:#cfefcf;" | '''Wide complex (QRS>0.12)''' | |||
|- | |||
! [[Supraventricular tachycardia with block]] | |||
| [[Image:atrial_tachy_with_LBBB_leadII.svg|200px|SVT with block - any SVT combined with LBBB or RBBB]] | |||
| (ir)regular depending on SVT | |||
| 100-250 bpm | |||
| 75-200 bpm | |||
| atria (SVT) | |||
| absent | |||
| temporary increased AV-block (eg 4:1) | |||
|- | |||
! [[AVRT|Atrio-ventricular Reentry Tachycardia (AVRT) - antidrome]] | |||
| | |||
| regular | |||
| 150-250 bpm | |||
| 150-250 bpm | |||
| circular: bypass - atria - av-node - ventricles | |||
| RP < PR | |||
| stops | |||
|- | |||
|} | |||
{{Box| | |||
===Supraventricular [[Ectopic Beats|ectopic beats]]=== | |||
*[[Atrial Premature Complexes]] | |||
*[[Wandering Pacemaker]] | |||
*[[AV-nodal complexes]] | |||
}} | }} | ||
{{Box| | |||
===Also read=== | |||
*[[Introduction to Arrhythmias]] | |||
*[[Mechanisms of Arrhythmias]] | |||
*[[Sinus node rhythms and arrhythmias]] | |||
*[[Junctional Tachycardias]] | |||
*[[Ventricular Arrhythmias]] | |||
{{ | |||
=== | |||
}} | }} | ||
{{Box| | |||
==References== | |||
<biblio> | |||
#ACC pmid=14563598 | |||
</biblio> | |||
{{ | |||
== | |||
# | |||
}} | }} | ||
[[Category:ECG Textbook]] | |||
Latest revision as of 19:09, 23 August 2011
| Author(s) | J.S.S.G. de Jong | |
| Moderator | J.S.S.G. de jong | |
| Supervisor | ||
| some notes about authorship | ||
Supraventricular tachycardias
|
|
|
| Arrhythmias are categorized into supraventricular and ventricular depending on their origin (below the bifurcation of the His bundle is ventricular) | An overview of pathological supraventricular arrhythmias and their origin | Algorithm to diagnose SVTs[1] |
|---|
| Example (lead II) | Regularity | Atrial frequency | Ventricular frequency | Origin (SVT/VT) | P-wave | Effect of adenosine | |
|---|---|---|---|---|---|---|---|
| Narrow complex (QRS<0.12) | |||||||
| Sinustachycardia | regular | 100-180 bpm | 100-180 bpm | sinusnode (SVT) | precedes every QRS complex | gradual slowing | |
| Atrial Fibrillation | grossly irregular | 400-600 bpm | 75-175 bpm | atria (SVT) | absent | slows down rate; irregularity remains | |
| Atrial Flutter | regular (sometimes alternating block) | 250-350 bpm | 75-150 bpm (3:1 or 2:1 block is most common) | atria (SVT) | negative sawtooth in lead II | temporary reduced conduction (e.g. 4:1) | |
| AVNRT | regular | 180-250 bpm | 180-250 bpm | AV-node (SVT) | in QRS complex (R') | stops | |
| Atrial Tachycardia | regular | 120-250 bpm | 75-200 bpm | atria | precedes QRS, p wave differs from sinus-p | temporary AV-block | |
| Atrio-Ventricular Reentry Tachycardia (AVRT)- orthodromic | regular | 150-250 bpm | 150-250 bpm | circle: av-node - ventricles - bypass - atria | RP < PR | stops | |
| AV junctional tachycardia | regular | 60-100 bpm | 70-130 bpm | AV node | RP < PR | reduces rate | |
| Wide complex (QRS>0.12) | |||||||
| Supraventricular tachycardia with block | (ir)regular depending on SVT | 100-250 bpm | 75-200 bpm | atria (SVT) | absent | temporary increased AV-block (eg 4:1) | |
| Atrio-ventricular Reentry Tachycardia (AVRT) - antidrome | regular | 150-250 bpm | 150-250 bpm | circular: bypass - atria - av-node - ventricles | RP < PR | stops | |
Supraventricular ectopic beats
References
- Blomström-Lundqvist C, Scheinman MM, Aliot EM, Alpert JS, Calkins H, Camm AJ, Campbell WB, Haines DE, Kuck KH, Lerman BB, Miller DD, Shaeffer CW, Stevenson WG, Tomaselli GF, Antman EM, Smith SC Jr, Alpert JS, Faxon DP, Fuster V, Gibbons RJ, Gregoratos G, Hiratzka LF, Hunt SA, Jacobs AK, Russell RO Jr, Priori SG, Blanc JJ, Budaj A, Burgos EF, Cowie M, Deckers JW, Garcia MA, Klein WW, Lekakis J, Lindahl B, Mazzotta G, Morais JC, Oto A, Smiseth O, Trappe HJ, and European Society of Cardiology Committee, NASPE-Heart Rhythm Society. ACC/AHA/ESC guidelines for the management of patients with supraventricular arrhythmias--executive summary. a report of the American college of cardiology/American heart association task force on practice guidelines and the European society of cardiology committee for practice guidelines (writing committee to develop guidelines for the management of patients with supraventricular arrhythmias) developed in collaboration with NASPE-Heart Rhythm Society. J Am Coll Cardiol. 2003 Oct 15;42(8):1493-531. DOI:10.1016/j.jacc.2003.08.013 |