Puzzle 2008 04 014 Answer: Difference between revisions
m (New page: {{NHJ| |mainauthor= '''N.J.W. Verouden, R.J. de Winter, A.A.M. Wilde''' |edition= 2009:01,062 }} Figure 1A|thumb [[Image:Puzzle_2008_04_014_fig1b.png...) |
mNo edit summary |
||
| Line 18: | Line 18: | ||
followed by a second ECG (figure 1B) 40 minutes | followed by a second ECG (figure 1B) 40 minutes | ||
later. | later. | ||
'''What would be your diagnosis and thoughts?''' | '''What would be your diagnosis and thoughts?''' | ||
==Answer== | ==Answer== | ||
The ECG in figure 1A shows sinus rhythm, an inter-mediate electrical axis, and a normal PQ interval and QRS duration. Furthermore, obvious ST-segmentelevation (STE) preceded by pathological Q waves inthe right precordial leads, STE in leads I and aVL, andreciprocal ST-segment depression in the inferior leads all imply an acute occlusion of the left anteriordescending (LAD) artery, located proximal to the firstseptal and first diagonal branch.<cite>Engelen</cite><cite>Tamura</cite> The recording in figure 1B reveals a regular rhythmwith broadened QRS complexes, likely a ventricular rhythm, of approximately 100 beats/min without visible atrial activation. The broadened QRS complexes(± 0.12 s) show a right bundle branch block (RBBB) configuration and a left anterior fascicular block, which causes the electrical axis to shift leftwards. Corrected QT intervals are normal. ST-segment shifts are com-parable to those in figure 1A. Both the left anterior fascicle and the right bundlebranch are supplied by septal branches of the proximal LAD artery. Ischaemia-induced bifascicular block, | The ECG in figure 1A shows sinus rhythm, an inter-mediate electrical axis, and a normal PQ interval and QRS duration. Furthermore, obvious ST-segmentelevation (STE) preceded by pathological Q waves inthe right precordial leads, STE in leads I and aVL, andreciprocal ST-segment depression in the inferior leads all imply an acute occlusion of the left anteriordescending (LAD) artery, located proximal to the firstseptal and first diagonal branch.<cite>Engelen</cite><cite>Tamura</cite> The recording in figure 1B reveals a regular rhythmwith broadened QRS complexes, likely a ventricular rhythm, of approximately 100 beats/min without visible atrial activation. The broadened QRS complexes(± 0.12 s) show a right bundle branch block (RBBB) configuration and a left anterior fascicular block, which causes the electrical axis to shift leftwards. Corrected QT intervals are normal. ST-segment shifts are com-parable to those in figure 1A. Both the left anterior fascicle and the right bundlebranch are supplied by septal branches of the proximal LAD artery. | ||
Ischaemia-induced bifascicular block, defined as RBBB along with left anterior (or posterior) fascicular block, has been associated with a 30% excessrisk of complete heart block and should therefore be regarded as ‘bad news’. Additional prolongation of the PR interval, known as incomplete trifascicular block, is associated with imminent high-degree AV block and temporary or permanent pacing used to be recommended in these circumstances in the days prior toprimary PCI.<cite>Hindman</cite><cite>Antman</cite><cite>Gregoratos</cite> | |||
In the pre thrombolytic era, in-hospitalmortality in these patients could be as high as 80%,which was mainly related to an extensive loss offunctioning myocardium.<cite>Hindman2</cite> In an emergency situation, a brief evaluation of theECG depicted in figure 1B could lead to the mis-diagnosis of a multifascicular conduction block causedby acute occlusion of the LAD artery. Nevertheless,and in contrary to the ECG in figure 1A, a normal Pwave or other forms of atrial pacemaker activity areabsent in this recording. Finally, the ECG recorded justprior to emergency coronary angiography (figure 2)shows both electrocardiographic appearances. We seethe transition from the regular ventricular rhythm intosinus rhythm with subsequent disappearance of RBBBconfiguration and left anterior fascicular block. | |||
In conclusion, it is most likely that an intermittentaccelerated idioventricular rhythm (AIVR) originatingfrom the left posterior fascicle caused the widened QRScomplex rhythm that competes with sinus rhythm. Asecond, less plausible explanation would be that theatrioventricular node or bundle of His were intermit-tently acting as the dominant pacemaker, accompaniedby ischaemia-induced conduction disturbance of theright bundle branch and left anterior fascicle, whichwould be an alarming sign of severe ischaemia affectingan extensive part of the myocardium.The emergency coronary angiography revealed anocclusion of the proximal LAD artery, which was successfully treated with primary percutaneous coronary intervention (PCI). | |||
==References== | ==References== | ||
<biblio> | <biblio> | ||
#Engelen PMID= | #Engelen PMID=10440150 | ||
#Tamura PMID= | #Tamura PMID=8541164 | ||
#Hindman PMID= | #Hindman PMID=688580 | ||
#Antman PMID= | #Antman PMID=18191746 | ||
#Gregoratos PMID= | #Gregoratos PMID=12379588 | ||
# | #Hindman2 PMID=688579 | ||
</biblio> | </biblio> | ||
Revision as of 16:01, 12 April 2008
| Author(s) | N.J.W. Verouden, R.J. de Winter, A.A.M. Wilde | |
| NHJ edition: | 2009:01,062 | |
| These Rhythm Puzzles have been published in the Netherlands Heart Journal and are reproduced here under the prevailing creative commons license with permission from the publisher, Bohn Stafleu Van Loghum. | ||
| The ECG can be enlarged twice by clicking on the image and it's first enlargement | ||
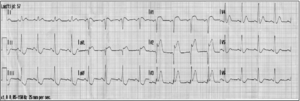
A 57-year-old man collapsed after one hour of angina symptoms in the presence of the alarmed ambulance personnel. He had never had any complaints of chest pain before and his medical history did not contain any cardiac events. Current smoking and a positive family history were noted as risk factors for coronary artery disease. Ventricular fibrillation (VF) was recorded as the first rhythm and the patient was successfully defibrillated with external DC shock. The first ECG after defibrillation is shown in figure 1A, followed by a second ECG (figure 1B) 40 minutes later.
What would be your diagnosis and thoughts?
Answer
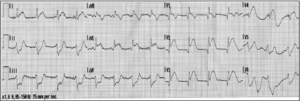
The ECG in figure 1A shows sinus rhythm, an inter-mediate electrical axis, and a normal PQ interval and QRS duration. Furthermore, obvious ST-segmentelevation (STE) preceded by pathological Q waves inthe right precordial leads, STE in leads I and aVL, andreciprocal ST-segment depression in the inferior leads all imply an acute occlusion of the left anteriordescending (LAD) artery, located proximal to the firstseptal and first diagonal branch.[1][2] The recording in figure 1B reveals a regular rhythmwith broadened QRS complexes, likely a ventricular rhythm, of approximately 100 beats/min without visible atrial activation. The broadened QRS complexes(± 0.12 s) show a right bundle branch block (RBBB) configuration and a left anterior fascicular block, which causes the electrical axis to shift leftwards. Corrected QT intervals are normal. ST-segment shifts are com-parable to those in figure 1A. Both the left anterior fascicle and the right bundlebranch are supplied by septal branches of the proximal LAD artery.
Ischaemia-induced bifascicular block, defined as RBBB along with left anterior (or posterior) fascicular block, has been associated with a 30% excessrisk of complete heart block and should therefore be regarded as ‘bad news’. Additional prolongation of the PR interval, known as incomplete trifascicular block, is associated with imminent high-degree AV block and temporary or permanent pacing used to be recommended in these circumstances in the days prior toprimary PCI.[3][4][5]
In the pre thrombolytic era, in-hospitalmortality in these patients could be as high as 80%,which was mainly related to an extensive loss offunctioning myocardium.[6] In an emergency situation, a brief evaluation of theECG depicted in figure 1B could lead to the mis-diagnosis of a multifascicular conduction block causedby acute occlusion of the LAD artery. Nevertheless,and in contrary to the ECG in figure 1A, a normal Pwave or other forms of atrial pacemaker activity areabsent in this recording. Finally, the ECG recorded justprior to emergency coronary angiography (figure 2)shows both electrocardiographic appearances. We seethe transition from the regular ventricular rhythm intosinus rhythm with subsequent disappearance of RBBBconfiguration and left anterior fascicular block.
In conclusion, it is most likely that an intermittentaccelerated idioventricular rhythm (AIVR) originatingfrom the left posterior fascicle caused the widened QRScomplex rhythm that competes with sinus rhythm. Asecond, less plausible explanation would be that theatrioventricular node or bundle of His were intermit-tently acting as the dominant pacemaker, accompaniedby ischaemia-induced conduction disturbance of theright bundle branch and left anterior fascicle, whichwould be an alarming sign of severe ischaemia affectingan extensive part of the myocardium.The emergency coronary angiography revealed anocclusion of the proximal LAD artery, which was successfully treated with primary percutaneous coronary intervention (PCI).
References
-
PMID=10440150
-
PMID=8541164
-
PMID=688580
-
PMID=18191746
-
PMID=12379588
-
PMID=688579