Puzzle 2007 6 231 Answer
| Author(s) | N.M. Panhuyzen-Goedkoop, L.R.C. Dekker, A.A.M. Wilde | |
| NHJ edition: | 2007:06,231 | |
| These Rhythm Puzzles have been published in the Netherlands Heart Journal and are reproduced here under the prevailing creative commons license with permission from the publisher, Bohn Stafleu Van Loghum. | ||
| The ECG can be enlarged twice by clicking on the image and it's first enlargement | ||
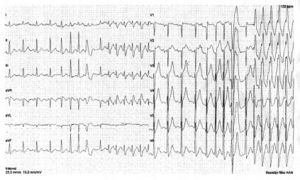
A 43-year-old man came to the outpatient clinic for preventive cardiovascular (CV) screening. During the last five years he complained of sudden onset of regular rapid palpitations during and after maximal exertion with dyspnoea. While holding his breath and working on abdominal muscular contractions he succeeded in ceasing these palpitations. This happened only a few times a year, but had been progressive in frequency and duration in the last six months. He had never collapsed during or after these palpitations. A cause had never been documented. His leisure time physical activity (6 hours/week) was long-distance running, fighting sports and fitness. There were no CV risk factors. His family history was negative. On physical examination his blood pressure was 125/85 mmHg, and there were no abnormal murmurs or heart sounds. Bicycle exercise testing (protocol 75 watts for five minutes, stepwise increment with 25 watts every minute) was normal (275 watts). Thereafter, a modified protocol starting at 75 watts for five minutes with instantaneous increase to 275 watts revealed the onset of a broad complex tachycardia (figure 1) with his usual symptoms. After ceasing and working on ‘his manoeuvre’ he managed to stop the tachycardia. In the 12-lead ECG the same episode is shown in the extremity leads (left side) and in the precordial leads (right side).
What is your diagnosis?
Answer
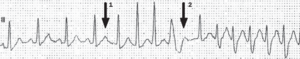
The first part of the ECG shows sinus rhythm with a regular rate of 130 beats/min. Four sinus P waves are followed by normal ventricular activation with a normal PR interval. The T wave of the 4th sinus beat is different to the preceding ones suggesting superimposement of a P wave (arrow 1 in figure 2 and very well seen in lead V1 of figure 1) which is subsequently conducted with a prolonged PR interval to the ventricle. A short supraventricular tachycardia (SVT) is initiated with a rate of 210 beats/min. A clear P wave is not observed in or related to the subsequent ventricular activation. After three beats a left bundle branch block (LBBB) complex is observed which might have been conducted from regular supraventricular activation. In the distal part of the ST segment, there is a clear sinus node P wave (figure 2, arrow 2) conducted through the atrioventricular node with a long PR interval, in turn followed by an RBBB tachycardia with the same frequency as the SVT shortly before.
In both cases the tachycardia is initiated by a prolonged PR interval which is highly suggestive of slow pathway conduction through the AV node. Hence, AV nodal reentrant tachycardia (AVNRT) is the most likely diagnosis in the second part of the ECG with aberrant conduction over the right bundle. The peculiarity in this ECG is the initiation of the second part by a sinus node beat (not a supraventricular extrasystole).
On invasive electrophysiological study AVNRT tachycardia was confirmed. Figure 3 shows two extremity leads, lead V1, five coronary sinus leads and recordings from the mapping catheter, which is in the right ventricle (100 mm/s). Two atrial extrasystoles are given (middle part of the recording) which conduct slowly to the ventricles and, on the right side of the recording, are followed by a spontaneous rhythm in which the QRS complex is immediately followed by the atrial depolarisation. This is highly suggestive of AV nodal reentrant tachycardia.
Conclusion: AVNRT induced by atrial extrasystoles and by a sinus beat. RBBB aberrant conduction. The LBBB beat is probably LBBB aberrant conduction or a ventricular extrasystole.