Pacemaker: Difference between revisions
mNo edit summary |
mNo edit summary |
||
| (49 intermediate revisions by 9 users not shown) | |||
| Line 1: | Line 1: | ||
{{ | {{authors| | ||
[[ | |mainauthor= [[user:Drj|J.S.S.G. de Jong]] | ||
[[ | |moderator= [[user:Drj|J.S.S.G. de jong]] | ||
|supervisor= | |||
}} | |||
{{clr}} | |||
{{Box| | |||
A pacemaker is indicated when electrical impulse conduction or formation is dangerously disturbed. The '''pacemaker rhythm''' can easily be recognized on the ECG. It shows '''pacemaker spikes''': vertical signals that represent the electrical activity of the pacemaker. Usually these spikes are more visible in unipolar than in bipolar pacing. | |||
In | In the first example, the atria are being paced, but not the ventricles, resulting in an '''atrial paced rhythm'''. Accordingly the ventricular complex is delayed until the atrial signal has passed through the AV node. In the second image the ventricles are paced directly, resulting in a '''ventricular paced rhythm'''. As ventricular pacing occurs exclusively in the right ventricle the ECG shows a left bundle branch block pattern. An exception to this rule is left ventricular pacing in patients with congenital anomalies and patients with surgically placed epicardial pacemakers. Another exception is septal or RVOT placement of the pacing lead, which results in a less widened to normal QRS complex. | ||
}} | |||
{{clr}} | |||
{|align="right" | |||
| | |||
[[Image:picture_pacemaker.jpg|thumb|A (used) DDDr pacemaker]] | |||
[[Image:chest_xray_pacemaker.jpg |thumb| Chest x-ray of a patient with a pacemaker]] | |||
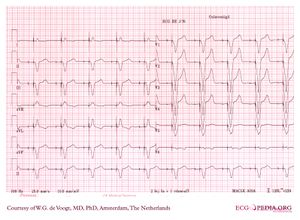
[[Image:paced2.gif|thumb| Ventricular paced rhythm shows ventricular pacemaker spikes]] | |||
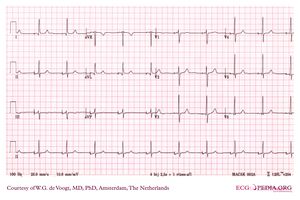
[[Image:ddd_paced_12lead.jpg |thumb| DDD paced rhythm]] | |||
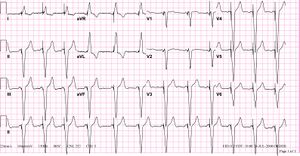
[[Image:Pacemaker2.jpg |thumb| Atrial sensed, ventricular paced rhythm (tracking). Note the LBBB morphology with left axis deviation indicating the pacing lead in the right ventricular apex.]] | |||
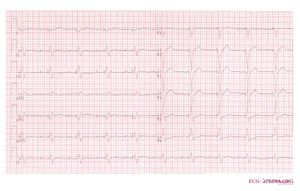
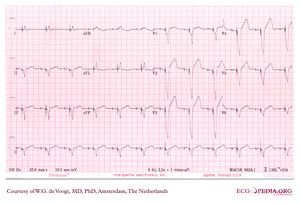
[[Image:DVA0838.jpg|thumb|Atrial paced rhythm]] | |||
|} | |||
==Pacemaker Coding== | |||
Pacemakers can be categorized according to the NASPE coding system, that usually consists of 3-5 letters. | |||
{| class="wikitable" width="80%" | |||
|+ '''The revised NASPE/BPEG generic code for antibradycardia pacing'''<cite>Bernstein</cite> | |||
! I || II || III || IV || V | |||
|- | |||
| Chamber(s) paced || Chamber(s) sensed || Response to sensing || Rate modulation || Multisite pacing | |||
|- | |||
| O = None || O = None || O = None || O = None || O = None | |||
|- | |||
| A = Atrium || A = Atrium || T = Triggered || R = Rate modulation || A = Atrium | |||
|- | |||
| V = Ventricle || V = Ventricle || I = Inhibited || || V = Ventricle | |||
|- | |||
| D = Dual (A+V) || D = Dual (A+V) || D = Dual (T+I) || || D = Dual (A+V) | |||
|- | |||
|} | |||
==Commonly Used Pacemakers== | |||
* AAI: | The most often used codes are: | ||
* VVI: | * '''AAI''': The atria are paced, when the intrinsic atrial rhythm falls below the pacemaker's threshold. | ||
* DDD: | * '''VVI''': The ventricles are paced, when the intrinsic ventricular rhythm falls below the pacemaker's threshold. | ||
* DDDR: | * '''VDD''': The pacemaker senses atrial and ventricular events, but can only pace the ventricle. This type of pacemaker is used in patients with a reliable sinus node, but with an AV-block. | ||
* | * '''DDD''': The pacemaker records both atrial and ventricular rates and can pace either chamber when needed. | ||
* ICD (Internal | * '''DDDR''': As above, but the pacemaker has a sensor that records a demand for higher cardiac output and can adjust the heart rate accordingly. | ||
* Biventricular pacemakers ('''CRT-P'''): Leads in both ventricles are present for synchronized contraction. The lead pacing the left ventricle is usually positioned in the coronary sinus. This cardiac resynchronization therapy can improve symptoms and survival in some heart failure patients. Several optimizing methods are being evaluated to find the most effective pacing delay between left and right ventricles. They include echocardiography, finding the narrowest QRS, and invasive hemodynamic measurements with pressure and flow wires. | |||
== | * '''[[ICD]]''' (Internal Cardioversion Device): This device can detect and treat [[Ventricular Tachycardia]] and [[Ventricular Fibrillation]]. ICDs are a separate category and usually not considered pacemakers although they do have a pacing function. Usually the first treatment is anti-tachy pacing (pacing at a rate +- 10% above the ventricular rate in ventricular tachycardia, which can convert the rhythm to sinus rhythm). If this is not effective, a defibrillator shock is delivered, usually with 16-36 Joules of energy. ICDs can save lives in patients who have a high risk of ventricular arrhythmias. All ICDs have optional pacemaker activity to treat bradycardias. New biventricular ICDs have 3 leads: an atrial lead, a left ventricular lead and a right ventricular lead. | ||
* Biventricular ICDs ('''CRT-D'''): an ICD with biventricular pacing option. | |||
{{clr}} | |||
==Pacemaker Indications== | |||
A full list of pacemaker indications can be read in the ESC guidelines on cardiac pacing <cite>Vardas</cite>. A selection of class I indications is: chronic symptomatic third- or second degree (Mobitz I or II) atrioventricular block, syncope with sinus node disease, alternating bundle branch block, and persisting AV block after surgery. | |||
===Atrial-sensed ventricular-paced rhythm=== | |||
===AV dual-paced rhythm=== | |||
[[Image:DVA0968.jpg|thumb|AV-sequencial paced rhythm]] | |||
{{clr}} | {{clr}} | ||
==Pacemaker Malfunction== | |||
====Failure of appropriate capture, atrial==== | |||
[[Image:DVA0856.jpg|thumb|Failure of atrial capture in a patient with atrial standstill, no P waves are seen after the atrial stimuli]] | |||
[[File:Atrial_capture_loss.svg|thumb|Loss of atrial capture]] | |||
{{clr}} | |||
====Failure of appropriate capture, ventricular==== | |||
[[File:ECG000020.jpg|thumb|Failure of ventricular capture]] | |||
[[File:Ventricular_noncapture.svg|thumb|Failure of ventricular capture]] | |||
{{clr}} | |||
====Failure of Appropriate Inhibition, Atrial==== | |||
Failure of appropiate inhibition results from atrial malsensing. | |||
[[File:atrial_malsensing.svg|thumb|Atrial malsensing. Atrial spikes are present right after spontaneous atrial activity.]] | |||
{{clr}} | |||
====Failure of Appropriate Inhibition, Ventricular==== | |||
[[File:Ventricular_undersensing.svg|thumb|Failure of Appropriate Ventricular Inhibition, ventricular undersensing]] | |||
====Failure of Appropriate Pacemaker Firing==== | |||
[[File:Ventricular_oversensing.svg|thumb|Failure of appropiate ventricular firing due to ventricular oversensing]] | |||
[[File:Atrial_malsensing.svg|thumb|Atrial malsensing]] | |||
====Retrograde Atrial Activation==== | |||
====Pacemaker Mediated Tachycardia==== | |||
[[Image:DVA1225.jpg|thumb|Pacemaker Mediated Tachycardia, successfully terminated by withholding a ventricular pace, followed by an atrial pace]] | |||
[[File:Pacemaker_mediated_tachycardia.svg|thumb|Pacemaker mediated tachycardia]] | |||
[[File:Termination_of_pmt.svg|thumb|Termination of pacemaker mediated tachycardia]] | |||
{{clr}} | |||
{{clr}} | |||
{{Box| | |||
==External Links== | |||
[http://www.hrsonline.org/swPositionStatementFiles/ps101036428.asp Heart Rhytm Society] | |||
}}{{clr}}{{Box| | |||
==References== | |||
<biblio> | |||
#Vardas pmid=17726042 | |||
#Gregoratos pmid=12379588 | |||
#Bernstein pmid=11916002 | |||
</biblio> | |||
}} | |||
{{clr}} | |||
[[Category:ECG Textbook]] | |||
Latest revision as of 17:32, 24 June 2010
| Author(s) | J.S.S.G. de Jong | |
| Moderator | J.S.S.G. de jong | |
| Supervisor | ||
| some notes about authorship | ||
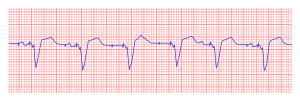
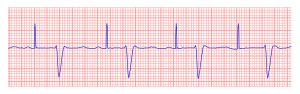
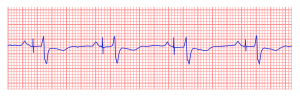
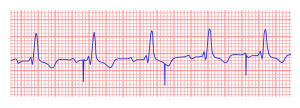
A pacemaker is indicated when electrical impulse conduction or formation is dangerously disturbed. The pacemaker rhythm can easily be recognized on the ECG. It shows pacemaker spikes: vertical signals that represent the electrical activity of the pacemaker. Usually these spikes are more visible in unipolar than in bipolar pacing.
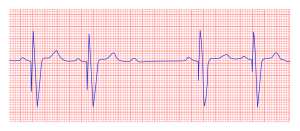
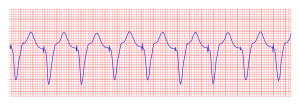
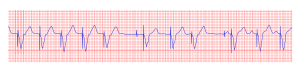
In the first example, the atria are being paced, but not the ventricles, resulting in an atrial paced rhythm. Accordingly the ventricular complex is delayed until the atrial signal has passed through the AV node. In the second image the ventricles are paced directly, resulting in a ventricular paced rhythm. As ventricular pacing occurs exclusively in the right ventricle the ECG shows a left bundle branch block pattern. An exception to this rule is left ventricular pacing in patients with congenital anomalies and patients with surgically placed epicardial pacemakers. Another exception is septal or RVOT placement of the pacing lead, which results in a less widened to normal QRS complex.
|
|
Pacemaker Coding
Pacemakers can be categorized according to the NASPE coding system, that usually consists of 3-5 letters.
| I | II | III | IV | V |
|---|---|---|---|---|
| Chamber(s) paced | Chamber(s) sensed | Response to sensing | Rate modulation | Multisite pacing |
| O = None | O = None | O = None | O = None | O = None |
| A = Atrium | A = Atrium | T = Triggered | R = Rate modulation | A = Atrium |
| V = Ventricle | V = Ventricle | I = Inhibited | V = Ventricle | |
| D = Dual (A+V) | D = Dual (A+V) | D = Dual (T+I) | D = Dual (A+V) |
Commonly Used Pacemakers
The most often used codes are:
- AAI: The atria are paced, when the intrinsic atrial rhythm falls below the pacemaker's threshold.
- VVI: The ventricles are paced, when the intrinsic ventricular rhythm falls below the pacemaker's threshold.
- VDD: The pacemaker senses atrial and ventricular events, but can only pace the ventricle. This type of pacemaker is used in patients with a reliable sinus node, but with an AV-block.
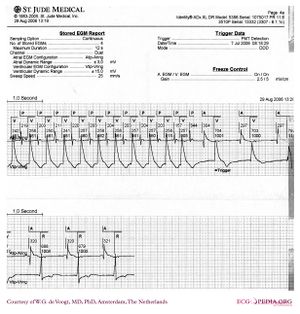
- DDD: The pacemaker records both atrial and ventricular rates and can pace either chamber when needed.
- DDDR: As above, but the pacemaker has a sensor that records a demand for higher cardiac output and can adjust the heart rate accordingly.
- Biventricular pacemakers (CRT-P): Leads in both ventricles are present for synchronized contraction. The lead pacing the left ventricle is usually positioned in the coronary sinus. This cardiac resynchronization therapy can improve symptoms and survival in some heart failure patients. Several optimizing methods are being evaluated to find the most effective pacing delay between left and right ventricles. They include echocardiography, finding the narrowest QRS, and invasive hemodynamic measurements with pressure and flow wires.
- ICD (Internal Cardioversion Device): This device can detect and treat Ventricular Tachycardia and Ventricular Fibrillation. ICDs are a separate category and usually not considered pacemakers although they do have a pacing function. Usually the first treatment is anti-tachy pacing (pacing at a rate +- 10% above the ventricular rate in ventricular tachycardia, which can convert the rhythm to sinus rhythm). If this is not effective, a defibrillator shock is delivered, usually with 16-36 Joules of energy. ICDs can save lives in patients who have a high risk of ventricular arrhythmias. All ICDs have optional pacemaker activity to treat bradycardias. New biventricular ICDs have 3 leads: an atrial lead, a left ventricular lead and a right ventricular lead.
- Biventricular ICDs (CRT-D): an ICD with biventricular pacing option.
Pacemaker Indications
A full list of pacemaker indications can be read in the ESC guidelines on cardiac pacing [2]. A selection of class I indications is: chronic symptomatic third- or second degree (Mobitz I or II) atrioventricular block, syncope with sinus node disease, alternating bundle branch block, and persisting AV block after surgery.
Atrial-sensed ventricular-paced rhythm
AV dual-paced rhythm
Pacemaker Malfunction
Failure of appropriate capture, atrial
Failure of appropriate capture, ventricular
Failure of Appropriate Inhibition, Atrial
Failure of appropiate inhibition results from atrial malsensing.
Failure of Appropriate Inhibition, Ventricular
Failure of Appropriate Pacemaker Firing
Retrograde Atrial Activation
Pacemaker Mediated Tachycardia
External Links
References
- Bernstein AD, Daubert JC, Fletcher RD, Hayes DL, Lüderitz B, Reynolds DW, Schoenfeld MH, and Sutton R. The revised NASPE/BPEG generic code for antibradycardia, adaptive-rate, and multisite pacing. North American Society of Pacing and Electrophysiology/British Pacing and Electrophysiology Group. Pacing Clin Electrophysiol. 2002 Feb;25(2):260-4. DOI:10.1046/j.1460-9592.2002.00260.x |
- Vardas PE, Auricchio A, Blanc JJ, Daubert JC, Drexler H, Ector H, Gasparini M, Linde C, Morgado FB, Oto A, Sutton R, Trusz-Gluza M, European Society of Cardiology, and European Heart Rhythm Association. Guidelines for cardiac pacing and cardiac resynchronization therapy: The Task Force for Cardiac Pacing and Cardiac Resynchronization Therapy of the European Society of Cardiology. Developed in collaboration with the European Heart Rhythm Association. Eur Heart J. 2007 Sep;28(18):2256-95. DOI:10.1093/eurheartj/ehm305 |
- Gregoratos G, Abrams J, Epstein AE, Freedman RA, Hayes DL, Hlatky MA, Kerber RE, Naccarelli GV, Schoenfeld MH, Silka MJ, Winters SL, Gibbons RJ, Antman EM, Alpert JS, Gregoratos G, Hiratzka LF, Faxon DP, Jacobs AK, Fuster V, Smith SC Jr, and American College of Cardiology/American Heart Association Task Force on Practice Guidelines/North American Society for Pacing and Electrophysiology Committee to Update the 1998 Pacemaker Guidelines. ACC/AHA/NASPE 2002 guideline update for implantation of cardiac pacemakers and antiarrhythmia devices: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/NASPE Committee to Update the 1998 Pacemaker Guidelines). Circulation. 2002 Oct 15;106(16):2145-61. DOI:10.1161/01.cir.0000035996.46455.09 |