Catecholaminergic Polymorphic Ventricular Tachycardia: Difference between revisions
Jump to navigation
Jump to search
mNo edit summary |
|||
| Line 36: | Line 36: | ||
#sumitomo pmid=12482795 | #sumitomo pmid=12482795 | ||
#Wilde pmid=18463378 | #Wilde pmid=18463378 | ||
#Collura pmid= | #Collura pmid=15642768 | ||
</biblio> | </biblio> | ||
Revision as of 18:35, 5 May 2010
| Author(s) | J.S.S.G. de Jong, MD | |
| Moderator | P.G. Postema, MD | |
| Supervisor | ||
| some notes about authorship | ||
Catecholaminergic Polymorphic Ventricular Tachycardia is a congenital disease that leads to exercise induced ventricular arrhythmias and / or syncope and carries an increased risk of sudden death.
Characteristics of CPVT:
- The mean onset of arrhythmias is 7-9 years
- Absence of structural cardiac abnormalities
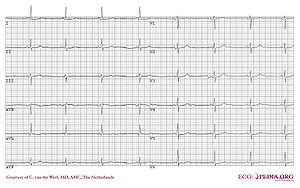
- Normal resting ECG
- Syncope during physical activity or emotional stress
Diagnosis
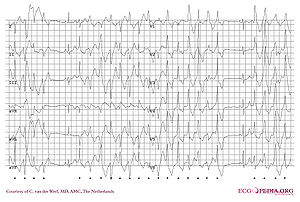
- The diagnosis is based on the patient's clinical history (dizziness or syncope induced by exercise or emotional stress and a family history containing syncope or sudden death in young relatives related to similar triggers) and reproducible ventricular arrhythmias during exercise testing. The complexity of these arrhythmias often increases with increasing work load, starting with Ventricular Premature Beats, and ending with bidirectional ventricular tachycardia to polymorphic ventricular tachycardia.
- Two genes have been linked to CPVT. Both lead to a defect in intracellular calcium metabolism:
Treatmentsumitomo
- Beta-blockers
- ICD implantation combined with beta-blockers in CPVT patients who survived a cardiac arrest or patients with syncope and/or documented sustained ventricular tachycardia despite beta-blocker therapy.ACC2006
- Surgical left cardiac sympathetic denervation in selected patients whose symptoms and/or ventricular arrhythmias are not controlled by pharmacologic therapy WildeCollura
- Avoid competitive and other strenuous exercise
External Links
References
<biblio>
- ACC2006 pmid=16935995
- sumitomo pmid=12482795
- Wilde pmid=18463378
- Collura pmid=15642768
</biblio>