Approach to the Wide Complex Tachycardia: Difference between revisions
| (18 intermediate revisions by 3 users not shown) | |||
| Line 1: | Line 1: | ||
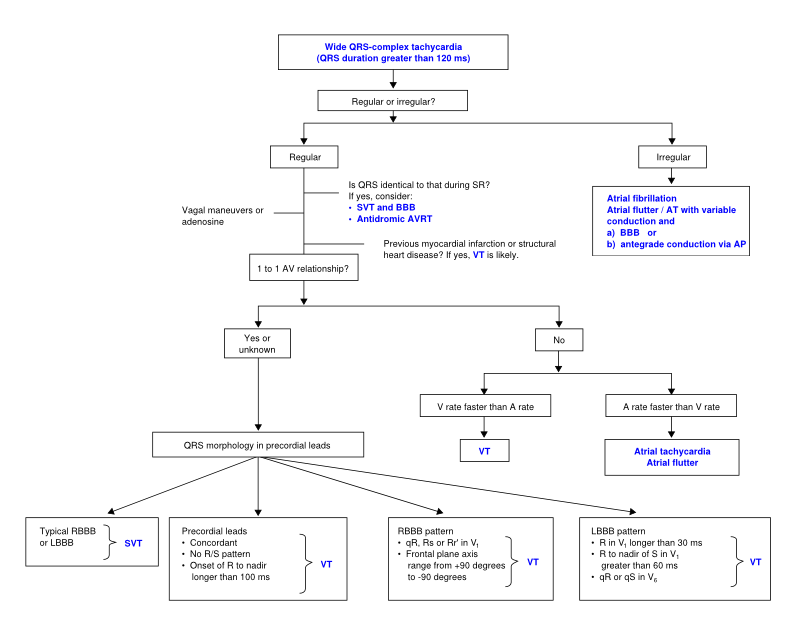
During wide complex tachycardia (heart rate > 100/min, QRS > 0.12 sec) the differentiation between supraventricular and ventricular origin of the arrhythmia is important to guide therapy. Several | During wide complex tachycardia (heart rate > 100/min, QRS > 0.12 sec) the differentiation between supraventricular and ventricular origin of the arrhythmia is important to guide therapy. Several algorithms have been developed to aid in this differentiation (below). It is important to keep in mind that a good estimate of VT ''versus'' SVT can be made based on the clinical vignette: | ||
* 'Horizontal entrance' into the ER. Older patient with previous myocardial infarction = most likely VT | * 'Horizontal entrance' into the ER. Older patient with previous myocardial infarction = most likely VT | ||
* Younger patient with known paroxysmal tachycardias and who is hemodynamically stable = most like SVT | * Younger patient with known paroxysmal tachycardias and who is hemodynamically stable = most like SVT | ||
== The ACC | == The ACC algorithm <cite>ACC</cite>== | ||
[[File: | [[File:VT_algorithm_en.svg|800px|thumb|left|SVT vs VT algorhytm. Adapted from <cite>ACC</cite>]] | ||
{{clr}} | {{clr}} | ||
== Brugada | ==ECG algorithms to differentiate wide QRS-complex tachycardias== | ||
[[ | Several ECG algorithms have been developed to differentiate wide QRS-complex tachycardias. Most of them performed very well in the population they were based upon. A recent review tested five commonly used algorithms in a control population and found that each of them only performed reasonably well in differentiating VT from SVT (accuracy 66-77%).<cite>Jastrzekbsi</cite> The five criteria tested were: | ||
* Brugada algorithm (below).<cite>Brug1</cite> This is the most commonly used algorithm. SN 89%, SP 59.2%. | |||
* The lead II R-wave-peak-time (below). <cite>Brugada2</cite> Sensitivity 60%, specificity 82.7%. | |||
* The aVR algorithm (below). <cite>Vereckei</cite> Sensitivity 87.1%, specificity 48%. | |||
* The Bayesian algorithm.<cite>Lau</cite> This calculates a score based on 19 morpologic features. Sensitivity 89%, specificity 52%. | |||
* The Griffith algorithm (below).<cite>Griffith</cite> Sensitivity 94.2%, specificity 39.8%. | |||
== Brugada algorithm == | |||
[[File:Brugada_algorithm.svg|500px|thumb|left]] | |||
{| class="wikitable" width="500px" | {| class="wikitable" width="500px" | ||
! colspan="3" | Morphological criteria (if the above criteria are inconclusive) | ! colspan="3" | Morphological criteria (if the above criteria are inconclusive) | ||
|- | |- | ||
| Line 46: | Line 43: | ||
|} | |} | ||
{{clr}} | {{clr}} | ||
== Ultrasimple Brugada criterion: RW to peak Time (RWPT) == | |||
[[File:RWPT.svg|thumb|right|300px|R-wave to Peak Time ≥ 50ms in lead II strongly suggests VT]]In 2010 Joseph Brugada et al. published a new criterion to differentiate VT from SVT in wide complex tachycardias: the R wave peak time in Lead II <cite>Brugada2</cite>. They suggest measuring the duration of onset of the QRS to the first change in polarity (either nadir Q or peak R) in lead II. If the RWPT is ≥ 50ms the likelihood of a VT very high (positive likelihood ratio 34.8). This criterion was successful in their own population of 163 selected patients and is awaiting prospective testing in a larger trial. | |||
{{clr}} | |||
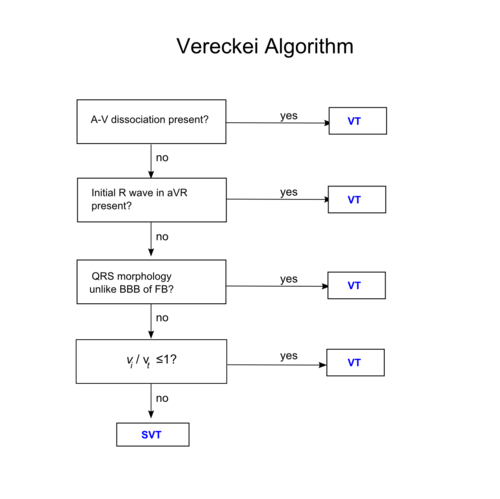
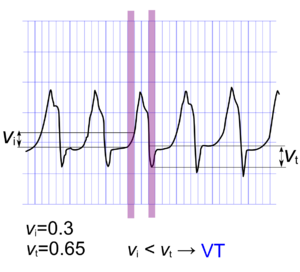
== Vereckei aVR algorithm <cite>Vereckei</cite>== | |||
[[File:Vereckei_algorithm.png|500px|thumb|left]] | |||
[[File:vivt.png|300px|thumb|If the distance traveled on the Y axis in the initial 40ms of the QRS complex is smaller than that traveled in the terminal 40ms of the QRS complex, a VT is much more likely]] | |||
{{clr}} | |||
== Griffith (Bundle Branch Block) algorithm == | |||
The Griffith algorithm <cite>Griffith</cite>reverses the diagnostic strategy: unless simple rules for a positive diagnosis of supraventricular tachycardia are satisfied, ventricular tachycardia is diagnosed by default. The algorithm only looks at bundle brach block morphology. Supraventricular tachycardia is diagnoses when ECG findings match typical bundle branch block: | |||
* LBBB: rS or QS wave in leads V1 and V2, delay to S wave nadir < 70 ms, and R wave and no Q wave in lead V6 | |||
* RBBB: rSR' wave in lead V1 and an RS wave in lead V6, with R wave height greater than S wave depth | |||
==Examples== | ==Examples== | ||
<gallery> | <gallery> | ||
Image:wide_qrs_tachy_AAM1.jpg|Wide complex tachycardia. No AV dissociation. RBBB. Resembles sinus rhythm from the same patient. | Image:wide_qrs_tachy_AAM1.jpg|Wide complex tachycardia. No AV dissociation. RBBB. Resembles sinus rhythm from the same patient. Conclusion: SVT with [[RBBB]] | ||
Image:wide_qrs_tachy_AAM2.jpg|ECG from the same patient in sinus rhythm. The QRS complex is very similiar. | Image:wide_qrs_tachy_AAM2.jpg|ECG from the same patient in sinus rhythm. The QRS complex is very similiar. | ||
Image:wide_qrs_tachy_AAM3.png|Wide complex tachycardia. LBBB configuration. Absence of RS in the chest leads. [[AV dissociation]] is present. Conclusion: [[VT]] | Image:wide_qrs_tachy_AAM3.png|Wide complex tachycardia. LBBB configuration. Absence of RS in the chest leads. [[AV dissociation]] is present. Conclusion: [[VT]] | ||
| Line 58: | Line 69: | ||
#ACC pmid=14563598 | #ACC pmid=14563598 | ||
#Brug1 pmid=2022022 | #Brug1 pmid=2022022 | ||
#Vereckei pmid=17272358 | |||
#Brugada2 pmid=20215043 | |||
#Jastrzekbsi pmid=22333239 | |||
#Lau pmid=11060873 | |||
#Griffith pmid=7905552 | |||
</biblio> | </biblio> | ||
Latest revision as of 19:01, 24 February 2013
During wide complex tachycardia (heart rate > 100/min, QRS > 0.12 sec) the differentiation between supraventricular and ventricular origin of the arrhythmia is important to guide therapy. Several algorithms have been developed to aid in this differentiation (below). It is important to keep in mind that a good estimate of VT versus SVT can be made based on the clinical vignette:
- 'Horizontal entrance' into the ER. Older patient with previous myocardial infarction = most likely VT
- Younger patient with known paroxysmal tachycardias and who is hemodynamically stable = most like SVT
The ACC algorithm ACC
ECG algorithms to differentiate wide QRS-complex tachycardias
Several ECG algorithms have been developed to differentiate wide QRS-complex tachycardias. Most of them performed very well in the population they were based upon. A recent review tested five commonly used algorithms in a control population and found that each of them only performed reasonably well in differentiating VT from SVT (accuracy 66-77%).Jastrzekbsi The five criteria tested were:
- Brugada algorithm (below).Brug1 This is the most commonly used algorithm. SN 89%, SP 59.2%.
- The lead II R-wave-peak-time (below). Brugada2 Sensitivity 60%, specificity 82.7%.
- The aVR algorithm (below). Vereckei Sensitivity 87.1%, specificity 48%.
- The Bayesian algorithm.Lau This calculates a score based on 19 morpologic features. Sensitivity 89%, specificity 52%.
- The Griffith algorithm (below).Griffith Sensitivity 94.2%, specificity 39.8%.
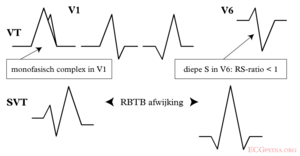
Brugada algorithm
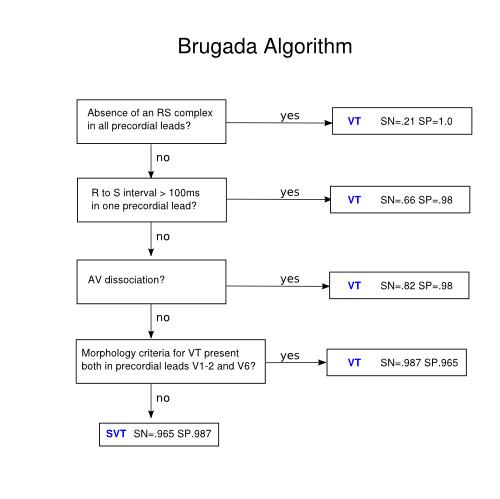
| Morphological criteria (if the above criteria are inconclusive) | ||
|---|---|---|
| LBBB pattern | ||
| Initial R more than 40ms? | Yes => VT |  |
| Slurred or notched downwards leg of S wave in leads V1 or V2 | Yes => VT | |
| Beginning of Q to nadir QS >60 ms in V1 or V2? | Yes => VT | LR >50:1 |
| Q or QS in V6? | Yes => VT | LR >50:1 |
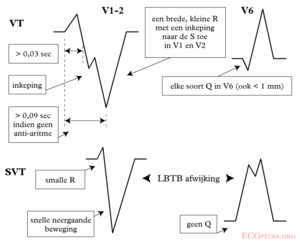 | ||
| RBBB pattern | ||
| Monofasic R or qR in V1? | Yes => VT | |
| R taller than R' (rabbit-ear sign)? | Yes => VT | LR >50:1 |
| rS in V6? | Yes => VT | LR >50:1 |
 | ||
Ultrasimple Brugada criterion: RW to peak Time (RWPT)
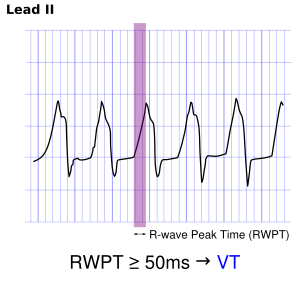
In 2010 Joseph Brugada et al. published a new criterion to differentiate VT from SVT in wide complex tachycardias: the R wave peak time in Lead II Brugada2. They suggest measuring the duration of onset of the QRS to the first change in polarity (either nadir Q or peak R) in lead II. If the RWPT is ≥ 50ms the likelihood of a VT very high (positive likelihood ratio 34.8). This criterion was successful in their own population of 163 selected patients and is awaiting prospective testing in a larger trial.
Vereckei aVR algorithm Vereckei
Griffith (Bundle Branch Block) algorithm
The Griffith algorithm Griffithreverses the diagnostic strategy: unless simple rules for a positive diagnosis of supraventricular tachycardia are satisfied, ventricular tachycardia is diagnosed by default. The algorithm only looks at bundle brach block morphology. Supraventricular tachycardia is diagnoses when ECG findings match typical bundle branch block:
- LBBB: rS or QS wave in leads V1 and V2, delay to S wave nadir < 70 ms, and R wave and no Q wave in lead V6
- RBBB: rSR' wave in lead V1 and an RS wave in lead V6, with R wave height greater than S wave depth
Examples
-
Wide complex tachycardia. No AV dissociation. RBBB. Resembles sinus rhythm from the same patient. Conclusion: SVT with RBBB
-
ECG from the same patient in sinus rhythm. The QRS complex is very similiar.
-
Wide complex tachycardia. LBBB configuration. Absence of RS in the chest leads. AV dissociation is present. Conclusion: VT
-
Wide complex tachycardia. LBBB configuration. Absence of RS in the chest leads. AV dissociation is present. Conclusion: VT
Referenties
<biblio>
- ACC pmid=14563598
- Brug1 pmid=2022022
- Vereckei pmid=17272358
- Brugada2 pmid=20215043
- Jastrzekbsi pmid=22333239
- Lau pmid=11060873
- Griffith pmid=7905552
</biblio>