ST Morphology
| «Step 6: QRS morphology | Step 7+1: Compare with previous ECG» |
| Author(s) | J.S.S.G. de Jong, MD | |
| Moderator | J.S.S.G. de Jong, MD | |
| Supervisor | ||
| some notes about authorship | ||
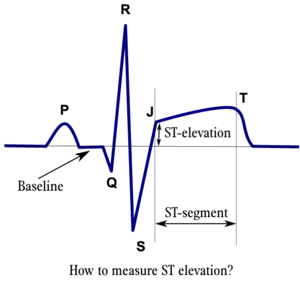
The ST segment represents ventricular repolarization. Repolarization follows upon contraction and depolarization. During repolarization the cardiomyocytes elongate and prepare for the next heartbeat. This process takes much more time than the depolarization. The elongation that takes place during repolarization is not passive; it is an active process during which energy is consumed. On the ECG, the repolarization phase starts at the junction, or j point, and continues until the T wave. The ST segment is normally at or near the baseline. Minor STT changes are not necessarily associated with cardiac ischemiaLloyd.
The T wave is usually concordant with the QRS complex. Thus if the QRS complex is positive in a certain lead (the area under the curve above the baseline is greater than the area under the curve below the baseline) than the T wave usually is positive too in that lead. Accordingly the T wave is normally upright or positive in leads I, II, AVL, AVF and V3-V6. The T wave is negative in V1 and AVR. The T wave flips around V2, but there is likely some genetic influence in this as in Blacks the T wave usually flips around V3.
The T wave angle is the result of small differences in the duration of the repolarization between the endocardial and epicardial layers of the left ventricle. The endocardial myocytes need a little more time to repolarize (about 22 msec). This difference causes an electrical current from the endocardium to the epicardium, which reads as a positive signal on the ECG.braunwald
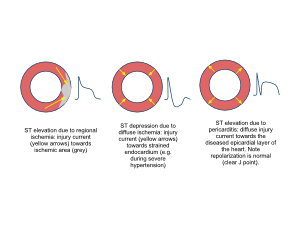
ST elevation
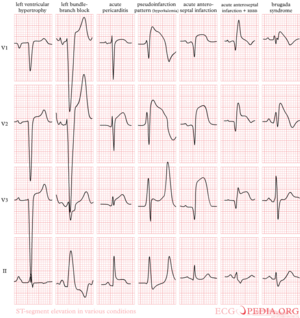
The most important cause of ST segment elevation is acute Ischemia. Other causes are WangWerf:
- Early repolarization
- Acute pericarditis: ST elevation in all leads except aVR
- Pulmonary embolism: ST elevation in V1 and aVR
- Hypothermia: ST elevation in V3-V6, II, III and aVF
- Hypertrophic cardiomyopathy: V3-V5 (sometimes V6)
- High potassium (hyperkalemia): V1-V2 (V3)
- During acute neurologic events: all leads, primarily V1-V6
- Acute sympathic stress: all leads, especially V1-V6
- Brugada syndrome.
- Cardiac aneurysm.
- Cardiac contusion
- Left ventricular hypertrophy
- Idioventricular rhythm including paced rhythm
In a study by Otto et al., among 123 patients with chest pain and ST segment elevation of >1mm, 63 patients did not have a myocardial infarction. Diagnoses in patients who did not have a myocardial infarction were LVH (33%) and LBBB (21%). Otto In daily practice this means that in these patients the diagnosis of myocardial infarction has to depend on other diagnostic means, such as laboratory tests, echocardiography and coronary angiography.
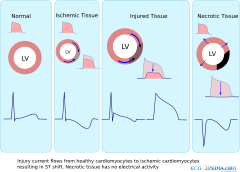
An important clue for the diagnosis of ischemia is the presence of reciprocal ST segment depression.

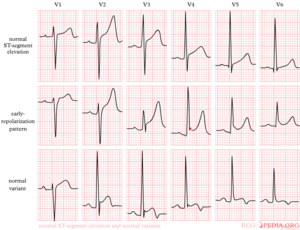
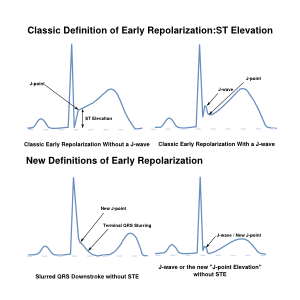
Early repolarization is a term used for ST segment elevation without underlying disease. It probably has nothing to do with actual early repolarization. It is commonly seen in young men. It is important to discern early repolarization from ST segment elevation from other causes such as ischemia. Characteristics of early repolarization are:Kambara
- an upward concave elevation of the RS-T segment with distinct or "embryonic" J waves
- slurred downstroke of R waves or distinct J points or both
- RS-T segment elevation commonly encountered in the precordial leads and more distinct in these leads
- rapid QRS transition in the precordial leads with counterclockwise rotation
- persistence of these characteristics for many years
- absence of reciprocal ST depression
- large symmetrical T waves
Recently early repolarization has also been used to describe late QRS notching or J wave slurring. When defined as such in the inferior leads (II, III en AVF) it has been found to be associated with an increased risk of cardiac death (1 mm of ST elevation carried an OR of 1.3 and 2 mm an OR of 3.0 )Tikkanen
ST depression
The most important cause of ST segment depression is Ischemia. Other causes of ST segment depression are:
- Reciprocal ST segment depression. If one lead shows ST segment elevation then usually the lead 'on the other side' shows ST segment depression. (This is usually seen in ischemia as well.
- Left ventricular hypertophy with "strain" or depolarization abnormality
- Digoxin effect
- Low potassium / low magnesium
- Heart rate-induced changes (post tachycardia)
- During acute neurologic events.
T wave changes


The T wave is quite 'labile' and long lists of possible causes of T wave changes exist. A changing T wave can be a sign that 'something' is abnormal, but it doesn't say much about the severity. T waves can be peaked, normal, flat, or negative. Flat and negative T waves are defined as:
- flat T wave
- < 0.5 mm negative or positive T wave in leads I, II, V3, V4, V5 or V6
- negative (or inverted) T wave
- > 0.5 mm negative T wave in leads I, II, V3, V4, V5 or V6
A concise list of possible causes of T wave changes:
- Ischemia and myocardial infarction
- Pericarditis
- Myocarditis
- Cardiac contusion
- Acute neurologic events, such as a subarachnoid bleed.
- Mitral valve prolapse
- Digoxin effect
- Right and left ventricular hypertrophy with strain
{{{1}}}