Supraventricular Rhythms
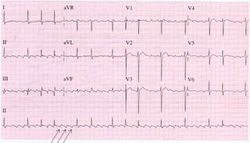
Sinustachycardia
| {{{locatieafbeelding}}} | |
| Atrial rate | 100-180 bpm |
| Ventricular rate | same |
| Regularity | {{{regularity}}} |
| Origin | sinus node |
| P-wave | positive in II, AVF |
| Effect of adenosine | no (can lead to temporary AV block) |
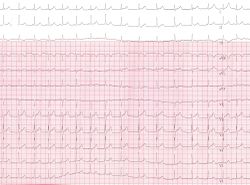
| Example ECG: | |
| Example ECG2: {{{example2}}} | |
In sinustachycardia the sinus node fires between 100 and 180 beats per minute and thus faster than normally. The maximal heartrate decreases with age from around 200 bpm to 140 bpm. The maximal heartrage can be estimated by subtracting the age in years from 210. Sinustachycardia normally has a gradual start and ending. Most often sinustachycardia is caused by an increase in the body's demand for oxygen, such as during exercise, stress, infection, blood loss and hyperthyroidism. It can also express an effort of the heart to compensate for a reduced stroke volume, as occurs during cardiomyopaty.
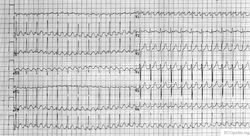
Atrial flutter
During atrial flutter the atria depolarize in an organized circular movement. This is caused by re-entry. The atria contract typically at around 300 bpm, which results in a fast sequence of p-waves in a sawtooth pattern on the ECG. For most AV-nodes this is way to fast to be able to conduct the signal to the ventricles, so typically there is a 2:1, 3:1 or 4:1 block, resulting in a ventricular frequency of 150, 100 or 75 bpm respectively. Often the grade of block changes every couple of beats, resulting in e.g. 2:1, or 3:1 blocks and a somewhat irregular ventricular heart rate. The saw-tooth is especially prominent in lead II, this lead normally shows constant electrical activity: it is never horizontal. Causes and risk of atrial flutter are comparable to atrial fibrillation.
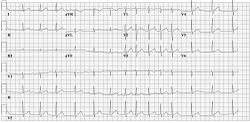
Atrial fibrillation
Main article: Atrial Fibrillation
During atrial fibrillation the atria show chaotic depolarisation with multiple foci. Mechanically the atria stop contracting after several days to weeks of atrial fibrillation, the result of the ultra-rapid depolarisations that occur in the atria, typically around 400 bpm, but up to 600 bpm. At the AV node 'every now and then' a beat is conducted to the ventricles, resulting in an irregular ventricular rate, which is the typical ECG characteristic of atrial fibrillation. Sometimes atrial fibrillation results in a course atrial flutter wave on the ECG, but the baseline can also be flat. A flat baseline is more often seen in long standing atrial fibrillation. The cardiac stroke volume is reduced by 10-20% during atrial fibrillation, as the 'atrial kick' is missing and because the heart does not have time to fill at the often higher ventricular rate. Causes; age (+- 10% of 70+ year olds and 15% of 90+ year olds have AFIB [1]), ischemia, hyperthyreoidism, alcohol abuse. Risc: thrombo-embolisation of thrombi that form in the atrial caverns as a result of the reduced atrial motion. These thrombi can emblise to the brain and cause strokes.
Atrial flutter can be catechorized as follows:
- First documented episode:
- Recurrent atrial fibrillation: after two or more episodes.
- Paroxysmal atrial fibrillation: if recurrent atrial fibrillation spontaneously converts to sinus rhythm.
- Persisting atrial fibrillation: if an episode of atrial fibrillation persists more than 7 days.
- Permanent atrial fibrillation: if atrial fibrillation persists after an effort of electrical or chemical cardioversion
Lone AF is atrial fibrillation in patients younger than 60 years in whom no clinical or electrocardiographic signs of heart or lung disease are present. These patiens have a favourable prognosis regarding thrombo-embolic events.
Non-valvular atrial fibrillation is atrial fibrillation in patients without heart valve disease or heart valve replacement or repair. [2]
Atrial Tachycardia
Atrial tachcyardia is a more or less regular heart rate > 100 bpm that does not origin from the sinus node. The p-waves therefore have a different configuration and easily be recognized if the are negative in AVF.
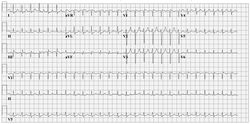
AVNRT
An AV Nodal Re-entry Tachycardia (AVNRT) is a rapid tachycardia with a typical frequency around 200 bpm. The tachycardia origin is the AV node. A prerequisite for AVNRT is a slow and fast pathway in the AV node, most often caused by degradation of the AV nodular tissue. The dual pathways facilitate re-entry.
Two sensitive characteristics to identify AVNRT on the ECG are:
- R'. This is a small secondary R wave. It resembles a right bundel branch block, but the QRS width stays < 120ms.
- RP << 100ms. The distance between the R and P waves is less than 100ms.
Atrio-ventricular Reentry Tachycardia AVRT
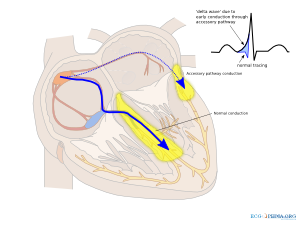
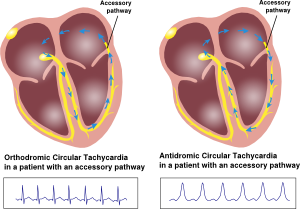
Atrio-ventricular Re-entry Tachycardias are somewhat similar to AVNRT. An important diffence however is that an accessory bundle is present in AVRT. This accessory bundle connects the atria and ventricles, thereby bypassing the AV node. The most common type of accessory bundle is a bundle of Kent. AVRTs can result from abnormal retrograde conduction (from ventricles to the atria) and anterorade conduction (from atria to ventricles). This results in two type of circular tachycardias:
- Orthodrome AV Re-entry Tachcardia (conduction retrogarde through the accessory bundle). Usually a narrow QRS complex preceded by a p-wave.
- Antidrome Atrioventricular Re-entry Tachcardia (anterogarde conduction through the abnormal accessory bundle). The ECG shows wide QRS complexes followed by retrograde P-waves. The RP-time is >> 100ms.
- Concealed Bypass Tract
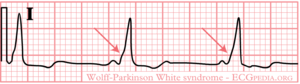
In 1930 Louis Wolff, Sir John Parkinson and Paul Dudley White described 11 patients who suffered from bouts of tachcyardias. Their ECGs showed two abnormalities: a short PQ time and a delta-wave.
Ever since one speaks of the Wolff-Parkinson-White syndrome in patients with complaints of syncope and / or tachycardia and a pre-exitation pattern on the ECG (WPW syndrome = WPW pattern + symptoms). Not all patients with a WPW pattern on the ECG are symptomatic. The prevalence of the WPW or pre-exitation pattern is relatively common in the general population (about 0.15-0.25%).
The pre-exitation pattern is caused by an extra connection between the atria and the ventricles (accessory bundle) that forms an electrical bypass to the AV node. The part of the ventricle where this accessory bundle connects are the first to depolarize. This is shown on the ECG as a delta wave. The QRS-complex is somewhat widened (> 0.10 sec). Also the PQ time is shorter (< 0.12 sec). By observing the pattern of the delta wave in the different leads, one can estimate the location of the accessory bundle.
The risk of having an accessory bundle is the development of tachycardias. Two forms of tachycardias exist:
- An atrioventricular tachcyardia, in which the electrical signal from the ventricles is conducted back to the atria. These fast arrhythmias (> 200 bpm) can deteriorate into ventricular fibrillation and sudden death.
- A supraventricular tachycardia with 1:1 conduction through the accessory bundle. A typical example is atrial fibrillation. Atrial fibrillation in WPW can result in a fast and irregular tachycardia: Fast, Broad & Irregular (FBI). This fast arrhythmia also carries the risk to deteriorate into ventricular fibrillation and sudden death.
In clinical practice it is therefore important to distinguish benign from malign accessory bundles.
Characteristics of a benign accessory bundle
- Intermittant WPW pattern on Holter registration
- Sudden disappearing of the pre-exitation pattern during exercise testing.
- The accessory bundle responds to blockade by medication (especially sodium channel blockers)
Characteristics of a malign accessory bundle
- The occurence of very fast arrhythmias during spontanous attacks of atrial fibrillation (> 240 bpm).
WPW can be treated by destroying the accessory bundle with ablation therapy.[3] Depending on the type of arrhythmias that occur anti-arrhythmic therapy can play a role.
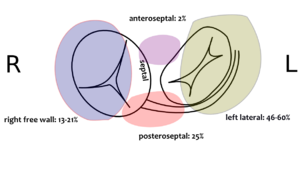
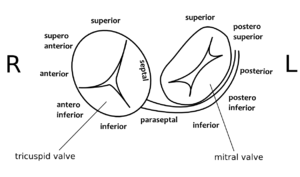
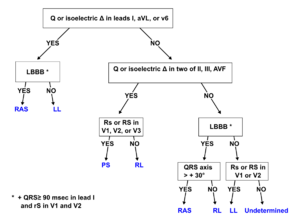
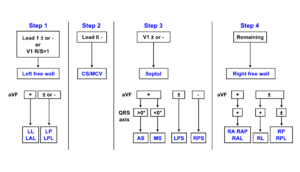
Determining the location of the accessory pathway
By closely observing the shape of the delta wave on the ECG, the location of the accessory connection can often be estimated. Several algorithms have been developed for this purpose.[4]
Examples
References
- Pappone C, Santinelli V, Manguso F, Augello G, Santinelli O, Vicedomini G, Gulletta S, Mazzone P, Tortoriello V, Pappone A, Dicandia C, and Rosanio S. A randomized study of prophylactic catheter ablation in asymptomatic patients with the Wolff-Parkinson-White syndrome. N Engl J Med. 2003 Nov 6;349(19):1803-11. DOI:10.1056/NEJMoa035345 |
- Milstein S, Sharma AD, Guiraudon GM, and Klein GJ. An algorithm for the electrocardiographic localization of accessory pathways in the Wolff-Parkinson-White syndrome. Pacing Clin Electrophysiol. 1987 May;10(3 Pt 1):555-63. DOI:10.1111/j.1540-8159.1987.tb04520.x |
- Cosío FG, Anderson RH, Becker A, Borggrefe M, Campbell RW, Gaita F, Guiraudon GM, Haïssaguerre M, Kuck KJ, Rufilanchas JJ, Thiene G, Wellens HJ, Langberg J, Benditt DG, Bharati S, Klein G, Marchlinski F, and Saksena S. Living anatomy of the atrioventricular junctions. A guide to electrophysiological mapping. A Consensus Statement from the Cardiac Nomenclature Study Group, Working Group of Arrythmias, European Society of Cardiology, and the Task Force on Cardiac Nomenclature from NASPE. North American Society of Pacing and Electrophysiology. Eur Heart J. 1999 Aug;20(15):1068-75. DOI:10.1053/euhj.1999.1657 |
- Arruda MS, McClelland JH, Wang X, Beckman KJ, Widman LE, Gonzalez MD, Nakagawa H, Lazzara R, and Jackman WM. Development and validation of an ECG algorithm for identifying accessory pathway ablation site in Wolff-Parkinson-White syndrome. J Cardiovasc Electrophysiol. 1998 Jan;9(1):2-12. DOI:10.1111/j.1540-8167.1998.tb00861.x |
AV junctional tachycardia