It's Not What You Think it Is: Difference between revisions
mNo edit summary |
Secretariat (talk | contribs) No edit summary |
||
| (2 intermediate revisions by one other user not shown) | |||
| Line 6: | Line 6: | ||
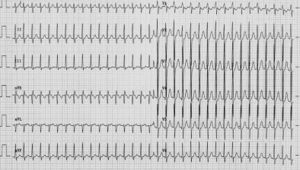
[[Image:Puzzle_2005_6_244_fig2.jpg|Figure 2|thumb]] | [[Image:Puzzle_2005_6_244_fig2.jpg|Figure 2|thumb]] | ||
A 20-year-old male is having palpitations. They | |||
occur without a specific trigger, although episodes | occur without a specific trigger, although episodes | ||
are sometimes related to emotion or exercise. Duration | are sometimes related to emotion or exercise. Duration | ||
| Line 30: | Line 30: | ||
treatment be?''' | treatment be?''' | ||
[[Answer]] | [[Puzzle 2005_6_244 - Answer|Answer]] | ||
Latest revision as of 14:02, 19 May 2010
| Author(s) | A.A.M. Wilde, R.B.A. van den Brink | |
| NHJ edition: | 2005:6,244 | |
| These Rhythm Puzzles have been published in the Netherlands Heart Journal and are reproduced here under the prevailing creative commons license with permission from the publisher, Bohn Stafleu Van Loghum. | ||
| The ECG can be enlarged twice by clicking on the image and it's first enlargement | ||
A 20-year-old male is having palpitations. They occur without a specific trigger, although episodes are sometimes related to emotion or exercise. Duration is between two minutes and one hour. He does not feel well during an attack, but has never fainted. Physical examination reveals no abnormalities nor does laboratory investigation or echocardiography. His baseline ECG is normal (not shown). He was asked to come to the emergency room if an episode lasted long enough, which he did (figure 1).
Upon presentation during an attack the ECG recorded a narrow-complex tachycardia with an RR interval of 280 msec (214 beats/min). There is a slight rightward deviation of the electrical axis. ST morphology is normal and no P wave can be identified. The differential diagnosis is:
- atrioventricular nodal reentry tachycardia (AVNRT),
- orthodromic tachycardia with a concealed bypass (AVRT) and
- atrial tachy-cardia. Adenosine was administered and the ECG presented in figure 2 was recorded.
What is your diagnosis and what would your further treatment be?