Atrial Fibrillation: Difference between revisions
mNo edit summary |
mNo edit summary |
||
| (26 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
{{Chapter|Supraventricular Rhythms}} | |||
{{Arrhythmias| | {{Arrhythmias| | ||
| name = Atrial fibrillation | | name = Atrial fibrillation | ||
| Line 6: | Line 7: | ||
| regularity = irregular | | regularity = irregular | ||
| origin = atria (SVT) | | origin = atria (SVT) | ||
| p_wave = | | p_wave = absent | ||
| adenosine = reduces heart rate | | adenosine = reduces heart rate | ||
}} | }} | ||
During atrial fibrillation the atria show chaotic depolarisation with multiple foci. Mechanically the atria stop contracting after several days to weeks of atrial fibrillation, the result of the ultra-rapid depolarisations that occur in the atria, typically around 400 bpm, but up to 600 bpm. At the AV node 'every now and then' a beat is conducted to the ventricles, resulting in an irregular ventricular rate, which is the typical ECG characteristic of atrial fibrillation. Sometimes atrial fibrillation results in a course atrial flutter wave on the ECG, but the baseline can also be flat. A flat baseline is more often seen in long standing atrial fibrillation. The cardiac stroke volume is reduced by 10-20% during atrial fibrillation, as the 'atrial kick' is missing and because the heart does not have time to fill at the often higher ventricular rate. Causes | {{#widget:Html5media | ||
|url=https://en.ecgpedia.org/images/a/a2/Atrial_Fibrillation.mp4 | |||
|width=640 | |||
|height=360 | |||
}} | |||
During atrial fibrillation the atria show chaotic depolarisation with multiple foci. Mechanically the atria stop contracting after several days to weeks of atrial fibrillation, the result of the ultra-rapid depolarisations that occur in the atria, typically around 400 bpm, but up to 600 bpm. At the AV node 'every now and then' a beat is conducted to the ventricles, resulting in an irregular ventricular rate, which is the typical ECG characteristic of atrial fibrillation. Sometimes atrial fibrillation results in a course atrial flutter wave on the ECG, but the baseline can also be flat. A flat baseline is more often seen in long standing atrial fibrillation. The cardiac stroke volume is reduced by 10-20% during atrial fibrillation, as the 'atrial kick' is missing and because the heart does not have time to fill at the often higher ventricular rate. | |||
'''Causes''' age (+- 10% of 70+ year olds and 15% of 90+ year olds have AFIB <cite>kelley</cite>), ischemia, hyperthyreoidism, alcohol abuse. | |||
'''Atrial fibrillation can be catechorized as follows:''' | '''Atrial fibrillation can be catechorized as follows:''' | ||
*'''First documented episode | *'''First documented episode''' | ||
*'''Recurrent atrial fibrillation:''' after two or more episodes. | *'''Recurrent atrial fibrillation:''' after two or more episodes. | ||
*'''Paroxysmal atrial fibrillation:''' if recurrent atrial fibrillation spontaneously converts to sinus rhythm. | *'''Paroxysmal atrial fibrillation:''' if recurrent atrial fibrillation spontaneously converts to sinus rhythm. | ||
| Line 23: | Line 28: | ||
''Non-valvular atrial fibrillation'' is atrial fibrillation in patients without heart valve disease or heart valve replacement or repair. <cite>ESCAF</cite> | ''Non-valvular atrial fibrillation'' is atrial fibrillation in patients without heart valve disease or heart valve replacement or repair. <cite>ESCAF</cite> | ||
'''Treatment strategies include:'''<cite>RACE</cite><cite>PIAF</cite><cite>STAF</cite> | |||
*''Rate control:'' accept atrial fibrillation and focus on symptom relief and prevention of tachycardias. Typically with beta-blockers and digoxin. Target rate is < 100 bpm. | |||
*''Rhythm control:'' trying to keep the patient in normal sinus rhythm. Typically with anti-arrhythmics like amiodarone, flecainide, and sotalol, or electrical cardioversion, or with radiofrequency catheter ablation. | |||
In both cases anti-coagulants are needed to prevent embolic stroke. | |||
{{clr}} | {{clr}} | ||
===References | ==Examples== | ||
<gallery caption:"Examples of atrial fibrillation"> | |||
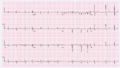
Image:afib_ecg.jpg|Atrial fibrillation with reasonable rate control | |||
Image:afib_f_VR_ecg.jpg|Atrial fibrillation with rapid ventricular rate | |||
Image:afib_detail.jpg|Detail of atrial fibrillation with rapid ventricular rate | |||
Image:cardioversion_from_afib.jpg|Atrial fibrillation electrically cardioverted into sinusrhythm | |||
Image:afib_V1.png|atrial fibrillation with marked organization in V1 (which is close to the right atrial appendage), this is not atrial flutter. | |||
</gallery> | |||
==References== | |||
<biblio> | <biblio> | ||
#ESCAF pmid=16885201 | #ESCAF pmid=16885201 | ||
#kelley pmid=17126661 | #kelley pmid=17126661 | ||
#RACE pmid=12466507 | |||
#PIAF pmid=11117910 | |||
#STAF pmid=12767648 | |||
</biblio> | </biblio> | ||
==External Links== | |||
[[w:Atrial Fibrillation|Wikipedia: Atrial Fibrillation]] | |||
Latest revision as of 21:14, 14 January 2021
| This is part of: Supraventricular Rhythms |
| {{{locatieafbeelding}}} | |
| Atrial rate | 400-600 bpm |
| Ventricular rate | 75-175 bpm |
| Regularity | irregular |
| Origin | atria (SVT) |
| P-wave | absent |
| Effect of adenosine | reduces heart rate |
| Example ECG: {{{example}}} | |
| Example ECG2: {{{example2}}} | |
During atrial fibrillation the atria show chaotic depolarisation with multiple foci. Mechanically the atria stop contracting after several days to weeks of atrial fibrillation, the result of the ultra-rapid depolarisations that occur in the atria, typically around 400 bpm, but up to 600 bpm. At the AV node 'every now and then' a beat is conducted to the ventricles, resulting in an irregular ventricular rate, which is the typical ECG characteristic of atrial fibrillation. Sometimes atrial fibrillation results in a course atrial flutter wave on the ECG, but the baseline can also be flat. A flat baseline is more often seen in long standing atrial fibrillation. The cardiac stroke volume is reduced by 10-20% during atrial fibrillation, as the 'atrial kick' is missing and because the heart does not have time to fill at the often higher ventricular rate. Causes age (+- 10% of 70+ year olds and 15% of 90+ year olds have AFIB [1]), ischemia, hyperthyreoidism, alcohol abuse.
Atrial fibrillation can be catechorized as follows:
- First documented episode
- Recurrent atrial fibrillation: after two or more episodes.
- Paroxysmal atrial fibrillation: if recurrent atrial fibrillation spontaneously converts to sinus rhythm.
- Persisting atrial fibrillation: if an episode of atrial fibrillation persists more than 7 days.
- Permanent atrial fibrillation: if atrial fibrillation persists after an effort of electrical or chemical cardioversion
Lone AF is atrial fibrillation in patients younger than 60 years in whom no clinical or electrocardiographic signs of heart or lung disease are present. These patiens have a favourable prognosis regarding thrombo-embolic events.
Non-valvular atrial fibrillation is atrial fibrillation in patients without heart valve disease or heart valve replacement or repair. [2]
Treatment strategies include:[3][4][5]
- Rate control: accept atrial fibrillation and focus on symptom relief and prevention of tachycardias. Typically with beta-blockers and digoxin. Target rate is < 100 bpm.
- Rhythm control: trying to keep the patient in normal sinus rhythm. Typically with anti-arrhythmics like amiodarone, flecainide, and sotalol, or electrical cardioversion, or with radiofrequency catheter ablation.
In both cases anti-coagulants are needed to prevent embolic stroke.
Examples
References
- Kelley GP, Stellingworth MA, Broyles S, and Glancy DL. Electrocardiographic findings in 888 patients > or =90 years of age. Am J Cardiol. 2006 Dec 1;98(11):1512-4. DOI:10.1016/j.amjcard.2006.06.055 |
- Fuster V, Rydén LE, Cannom DS, Crijns HJ, Curtis AB, Ellenbogen KA, Halperin JL, Le Heuzey JY, Kay GN, Lowe JE, Olsson SB, Prystowsky EN, Tamargo JL, Wann S, Task Force on Practice Guidelines, American College of Cardiology/American Heart Association, Committee for Practice Guidelines, European Society of Cardiology, European Heart Rhythm Association, and Heart Rhythm Society. ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation-executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Revise the 2001 Guidelines for the Management of Patients with Atrial Fibrillation). Eur Heart J. 2006 Aug;27(16):1979-2030. DOI:10.1093/eurheartj/ehl176 |
- Van Gelder IC, Hagens VE, Bosker HA, Kingma JH, Kamp O, Kingma T, Said SA, Darmanata JI, Timmermans AJ, Tijssen JG, Crijns HJ, and Rate Control versus Electrical Cardioversion for Persistent Atrial Fibrillation Study Group. A comparison of rate control and rhythm control in patients with recurrent persistent atrial fibrillation. N Engl J Med. 2002 Dec 5;347(23):1834-40. DOI:10.1056/NEJMoa021375 |
- Hohnloser SH, Kuck KH, and Lilienthal J. Rhythm or rate control in atrial fibrillation--Pharmacological Intervention in Atrial Fibrillation (PIAF): a randomised trial. Lancet. 2000 Nov 25;356(9244):1789-94. DOI:10.1016/s0140-6736(00)03230-x |
- Carlsson J, Miketic S, Windeler J, Cuneo A, Haun S, Micus S, Walter S, Tebbe U, and STAF Investigators. Randomized trial of rate-control versus rhythm-control in persistent atrial fibrillation: the Strategies of Treatment of Atrial Fibrillation (STAF) study. J Am Coll Cardiol. 2003 May 21;41(10):1690-6. DOI:10.1016/s0735-1097(03)00332-2 |