Test
| «Introduction | Step 1: Heart Rate» |
| Author(s) | I.A.C. van der Bilt, MD | |
| Moderator | I.A.C. van der Bilt, MD | |
| Supervisor | ||
| some notes about authorship | ||
How do I begin to read an ECG?
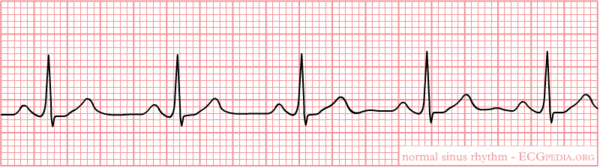
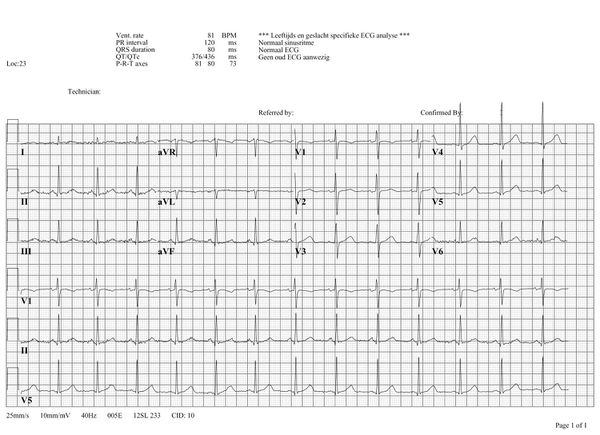
Click on the ECG to see an enlargement. Where do you start when interpreting an ECG?
- on the top left are the patient's information, name, sex and date of birth
- at the right of that are below each other the Frequency, the conduction times (PQ,QRS,QT/QTc), and the heart axis (P-top axis, QRS axis and T-top axis)
- further to the right is the interpretation of the ECG written (this often misses in a 'fresh' ECG, but later the interpretation of the cardiologist or computer will be added)
- down left is the 'paper speed' (25 mm/s on the horizontal axis), the sensitivity (10mm/mV) and the filter's frequency (40Hz, filters noise from eg. lights)
- finally there is a calibration on the ECG, on the beginning of every lead is a vertical block that shows with what amplitude a 1 mV signal is drawn. So the height and depth of these signals are a measurement for the voltage. If this is not the set at 10 mm, there is something wrong with the machine setting.
- further we have the ECG leads themselves of course, these will be discussed below.
Note that the lay-out is different for every machine, but most machines will show the information above somewhere.
What does the ECG register?
- The electrocardiogram
- An electrocardiogram (ECG or EKG) is a registration of the heart's electric activity.
Just like skeletal muscles, the heart is electrically stimulated to contract. This stimulation is also called activation or excitation. Cardiac muscles are electrically charged at rest. The inside of the cell is negatively charged relative to the outside (resting potential). If the cardiac muscle cells are electrically stimulated they depolarize (the resting potential changes from negative to positive) and contract. The electrical activity of a single cell can be registered as the action potential. As the impulse spreads through the heart, the electric field changes continually in size and direction. The ECG is a graphical visualisation of these electric signals in the heart.
The ECG represents the sum of the action potentials of millions of cardiomyocytes
The individual action potentials of the individual cardiomyocytes are averaged. The final result which is shown on the ECG is actually the average of trillions of microscopic electronical signals.
| height=350px|width=400px</flashow> |
| This movie shows the contraction of a single (rabbit) heart cell. The glass electrode measures the electrical current in the heart cell (with thepatch-clamp method). The electrical signal is written in blue and shows the actionpotential. Courtesy of Arie Verkerk and Antoni van Ginneken, AMC, Amsterdam, The Netherlands. |
The electric discharge of the heart
| height=300px</flashow> |
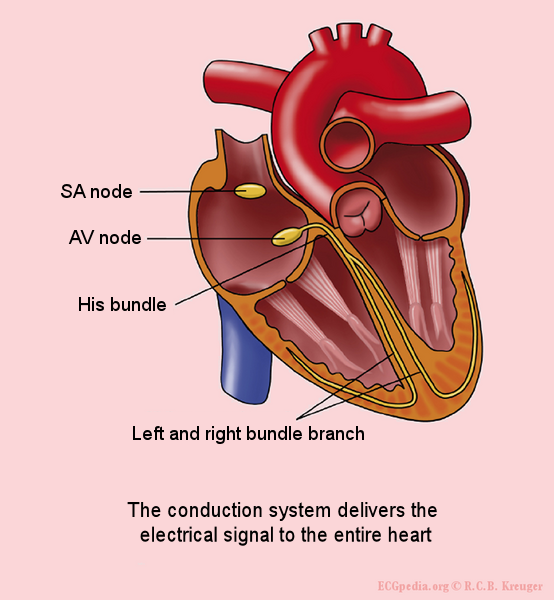
The sinal node (SA node) contains pacemakercells which determine the heart frequency.
First the atria depolarise and contract, after that the ventricles
The electrical signal between the atria and the ventricles goes from the sinus node, via the atria to the AV-node (atrioventricular transition) to the His bundle and subsequently to the right and left bundle branch, which end in a dense network of Purkinje fibers.
The different ECG waves
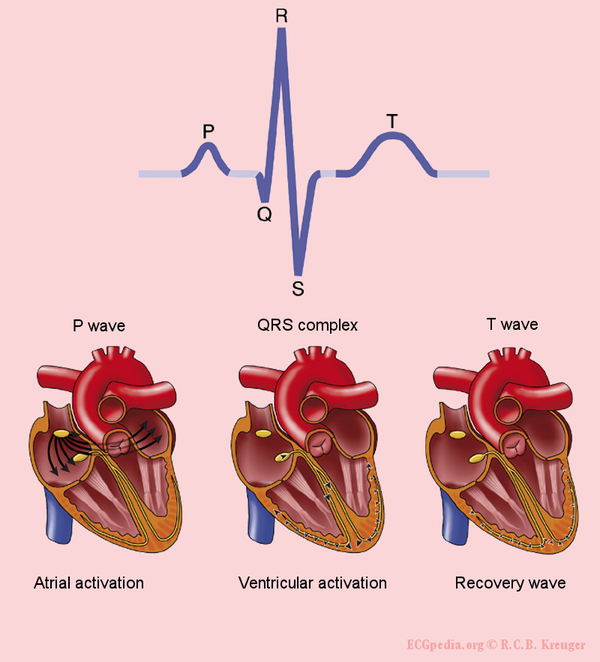


The P wave is the result of the atrial depolarization. This depolarization starts in the SA (sino-atrial) node. The signal produces by pacemakercells in the SA node is conducted by the conduction system to the right and left atria. Normal atrial repolarisation is not visible on the ECG (but can be visible during atrial infarction and pericarditis).
The QRS complex is the average of the depolarization waves of the inner (endocardial) and outer (epicardial) cardiomyocytes. As the endocardial cardiomyocytes depolarize slightly earlier than the outer layers, a typical QRS pattern occurs (figure).
The T wave represents the repolarisation of the ventricles. There is no cardiac muscle activity during the T wave.
One heart beat consists of an atrial depolarization --> atrial contraction --> p-wave, ventricular depolarization --> ventricular contraction --> ORS-complex and the resting phase (including the repolarization during the T-wave) between two heart beats.
Have a look at this excellent [animation of the heart cycle]
The origin of the U wave is unknown. This wave possibly results from "afterdepolarizations" of the ventricles.
The letters "Q", "R" and "S" are used to describe the QRS complex:
- Q: the first negative deflection after the p-wave. If the first deflection is not negative, the Q is absent.
- R: the positive deflection
- S: the negative deflection after the R-wave
- small print letters (q, r, s) are used to describe deflections of small amplitude. For example: qRS = small q, tall R, deep S.
- R`: is used to describe a second R-wave (as in a right bundlebranch block)
See figure for some examples of this.
The history of the ECG
A concise history of the ECG is presented in a different chapter.
The ECG electrodes

Electric activity going through the heart, can be measured by external (skin)electrodes. The electrocardiogram (ECG) registers these activities from these electrodes which have been attached on different places on the body. In total, twelve leads are calculated using ten electrodes.
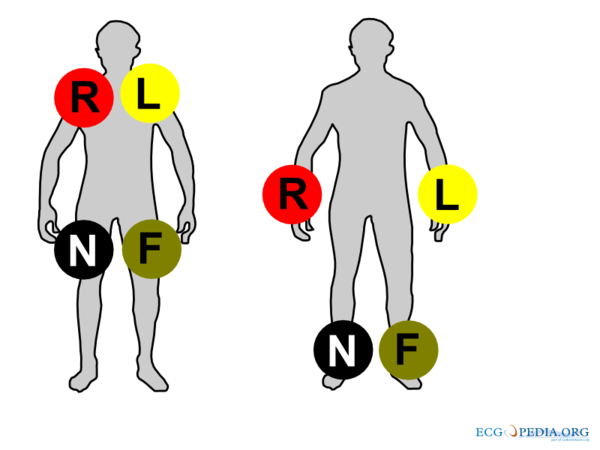
The ten electrodes are:
- the extremity electrodes:
- LA - left arm
- RA - right arm
- N - neutral, on the right leg (= electrical earth or point zero to which the electrical current is measured)
- F - foot, on the left leg
It makes no difference whether the electrodes are attached proximal or distal on the extremities. However, it is best to be uniform in this. (eg. do not attach an electrode on the left shoulder and one on the right wrist).
- the chest electrodes:
- V1 - placed in the 4th intercostal space, right of the sternum
- V2 - placed in the 4th intercostal space, left of the sternum
- V3 - placed between V2 and V4
- V4 - placed 5th intercostal space in the nippleline. Official recommendations are to place V4 under the breast in women.Kligfield
- V5 - placed between V4 and V6
- V6 - placed in the midaxillary line on the same height as V4 (horizontal line from V4, so not necessarily in the 5th intercostal space)
Using these 10 electrodes, 12 leads can be derived. There are 6 extremity leads and 6 precordial leads.
The Extremity Leads

The extremity leads are:
- I from the right to the left arm
- II from the right arm to the left leg
- III from the left arm to the left leg
An easy rule to remember: lead I + lead III = lead II This is done with the use of the height or depth, independent of the wave (QRS, P of T). Example: if in lead I, the QrS complex is 3 mm in height and in lead III 9mm, the height of the QRS-complex in lead II is 12mm.
Other extremity leads are:
- AVL points to the left arm
- AVR points to the right arm
- AVF points to the feet
The capital A stands for "augmented" and V for "voltage".
(aVR + aVL + aVF = 0)
The Chest Leads
The precordial, or chestleads, (V1,V2,V3,V4,V5 and V6) 'observe' the depolarization wave in the frontal plane
Example: V1 is close to the right ventricle and the right atrium. Signals in these areas of the heart have the largest signal in this lead. V6 is the closest to the lateral wall of the left ventricle.
Special Leads
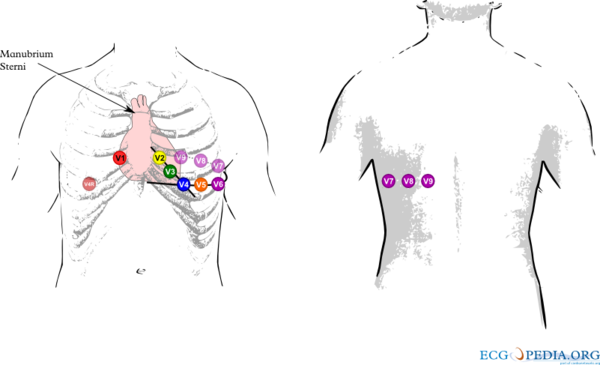
In case of an inferior wall infarct, extra leads may be used:
- In a right side ECG, V1 and V2 remain on the same place.V3 to V6 are placed on the same place but mirrored on the chest. So V4 is in the middle of the right clavicle. On the ECG it should be marked that it is a Right sided ECG. V4R (V4 but right sided) is a sensitive lead to diagnose right ventricular infarction.
- Leads V7-V8-V9 can be used to diagnose a posteriorinfarct. It is means that after V6, leads are placed towards the back. See the chapterIschemia for other ways of diagnosing posterior infarction.
| Author(s) | J.S.S.G. de Jong | |
| Moderator | J.S.S.G. de Jong | |
| Supervisor | ||
| some notes about authorship | ||
Lead reversals
Lead switches are a common mistake when ECGs are made and can lead to wrong diagnoses. Common mistakes are:
- Left-right arm reversals lead to a negative complex in lead I with a negative P wave in lead I. They are one of the most common causes of right axis deviation on the ECG!
- Arm-foot switches lead to a very small or 'far field' signal in leads II or III.
- Chest lead reversals lead to inappropriate R wave progression (increase-decrease-increase) and are often easily recognized.
Therefore any right axis or small signal in an extremity lead should be reason enough to check lead positioning. A previous ECG can be very helpful.
More specific patterns with every lead reversal:
- right and left arm electrodes:
- inversion of lead I
- reversal of leads II and III
- reversal of leads aVR and aVL
- right leg and right arm:
- diminished signal in lead II
- left arm and left leg:
- reversal of leads I and II
- reversal of leads aVL and aVF
- inversion of lead III
- right arm and left leg:
- inversion of leads I, II and III
- reversal of leads aVR and aVF
It is possible to distinguish lead reversal and dextrocardia by watching the precordial leads. Dextrocardia will not show any R wave progression in leads V1-V6, whereas lead reversal will.
-
Right and left arm lead reversal can be distinguished from the (much rarer) dextrocardia by examination of the precordial R wave progression.
-
Right arm and left leg lead reversal. Lead II now measures the signal between the left and right leg, which is remote from the heart.
-
A patient with dextrocardia (and previous inferior myocardial infarction)
-
Another patient with dextrocardia
Artifacts
Artifacts (disturbances) can have many causes. Common causes are:
- Movement
- Electrical interference
Filter settings
Although not a technical problem, filter settings influence the interpretation of the ECG.Garcia
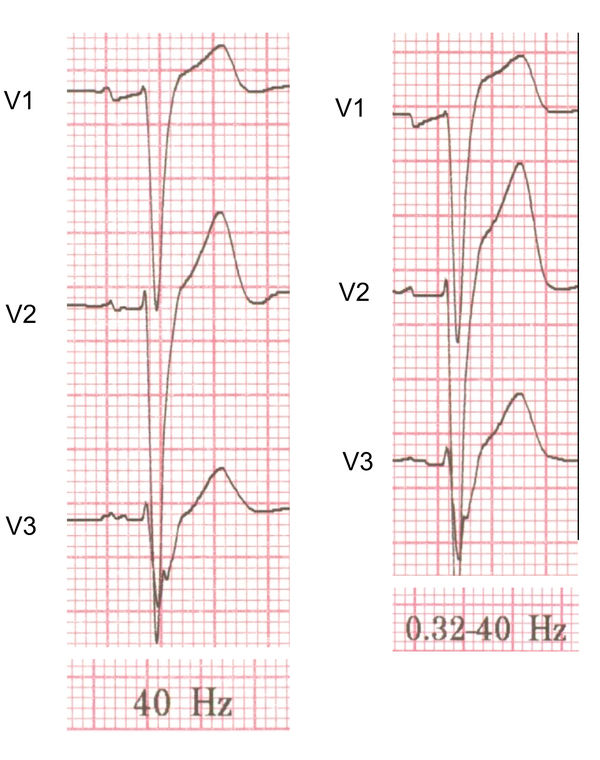
To reduce electrical interference ECG machine use two filters:
- A high-pass filter reduces low frequency noise. This filter reduces base line drift on the ECG.
- A low-pass filter reduces high frequency noise, such as produces by chest and extremity muscles and electrical interference from the power grid.
Depending on the purpose of the ECG these filters can be adjusted.
- In the monitor mode the high-pass filter can be set higher at 0.5-1.0 Hz and the low-pass filter on 40 Hz. This is the strongest filter setting (only a narrow frequency range is passed by the filter). This setting is especially useful for rhythm monitoring where noise can be distracting and ST segment interpretation is not very important. In this mode, pacemakerspikes are sometimes invisible while filtered out.
- In the diagnostic mode the high-pass filter is set at 0.05 Hz and the low-pass filter at 40, 100 or 150 Hz. This improves the diagnostic accuracy of the ST semgent. On the downside a base line drift occurs more easily.
-
Movement artifacts
-
Increasing movement artifacts in a Parkinson's patient. The patient was in sinus rhythm (which doesn't show on this short recording)!
-
Baseline drift. The amplifier in the ECG machine has to re-find the 'mean'. This often occurs right after lead connection and after electric cardioversion.
-
Cardioversion from atrial fibrillation to sinus rhythm, with clear baseline drift.
-
Electrical interference from a nearby electrical appliance. A typical example is a 100 Hz background distortion from fluorescent lights. Not to be confused with atrial fibrillation.
-
Another example of an artifact caused by an electrical appliance. The patients rhythm is regular. This strip shows 10 QRS complexes.
-
An artifact that was originally diagnosed as a VT
References
<biblio>
- Garcia pmid=19804517
</biblio>
References
<biblio>
- Dubois Du Bois-Reymond, E. Untersuchungen über thierische Elektricität. Reimer, Berlin: 1848.
- Hoffa Hoffa M, Ludwig C. 1850. Einige neue versuche uber herzbewegung. Zeitschrift Rationelle Medizin, 9: 107-144
- Waller Waller AD. A demonstration on man of electromotive changes accompanying the heart's beat. J Physiol (London) 1887;8:229-234
- Einthoven Einthoven W. Le telecardiogramme. Arch Int de Physiol 1906;4:132-164
- Einthoven2 Einthoven W. Über die Form des menschlichen Electrocardiogramms. Pfügers Archiv maart 1895, pagina 101-123
- Marey Marey EJ. Des variations electriques des muscles et du couer en particulier etudies au moyen de l'electrometre de M Lippman. Compres Rendus Hebdomadaires des Seances de l'Acadamie des sciences 1876;82:975-977
- Marquez pmid=12177632
- Hurst pmid=9799216
- Kligfield pmid=17322457
</biblio>