Pacemaker: Difference between revisions
No edit summary |
|||
| Line 56: | Line 56: | ||
to be filled in ... | to be filled in ... | ||
====Failure of appropriate capture, atrial==== | ====Failure of appropriate capture, atrial==== | ||
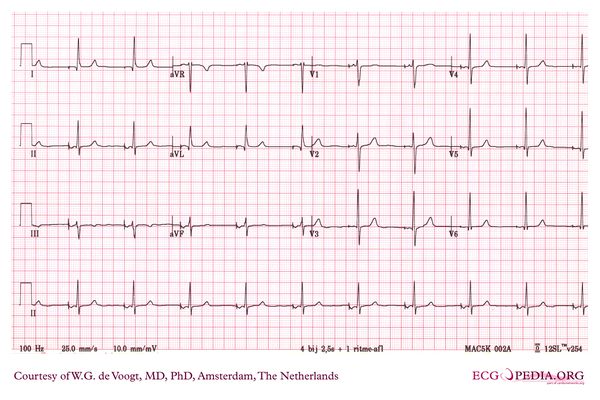
[[Image:DVA0856.jpg|thumb|Failure of atrial capture in a patient with atrial standstill, no P waves are seen after the atrial stimuli]] | |||
====Failure of appropriate capture, ventricular==== | ====Failure of appropriate capture, ventricular==== | ||
====Failure of appropriate inhibition, atrial==== | ====Failure of appropriate inhibition, atrial==== | ||
Revision as of 15:04, 29 November 2008
| Author(s) | J.S.S.G. de Jong | |
| Moderator | J.S.S.G. de jong | |
| Supervisor | ||
| some notes about authorship | ||




A pacemaker is indicated when the electrical impulse conduction or formation is dangerously disturbed. The paced pacemaker rhythm can easily be recognized on the ECG as it shows pacemaker spikes: vertical signals that represent the electrical activity of the pacemaker.
In the first example image, the atria are being paced, but not the ventricles, resulting in a atrial paced rhythm. Accordingly the ventricular beat is delayed until the atrial signal has passed the AV node. In the second image the ventricles are paced directly, resulting in ventricular paced rhythm. As ventricular pacing occurs exclusively in the right ventricle the ECG shows a left bundle branch pattern. An exception to this rule is left ventricular pacing in patients with congenital anomalies and patients with an epicardial pacemaker that has been placed during surgery.
Pacemaker Coding
Pacemakers can be categorized according to the NASPE coding system, that usually consists of 3-5 letters.
| I | II | III | IV | V |
|---|---|---|---|---|
| Chamber(s) paced | Chamber(s) sensed | Response to sensing | Rate modulation | Multisite pacing |
| O = None | O = None | O = None | O = None | O = None |
| A = Atrium | A = Atrium | T = Triggered | R = Rate modulation | A = Atrium |
| V = Ventricle | V = Ventricle | I = Inhibited | V = Ventricle | |
| D = Dual (A+V) | D = Dual (A+V) | D = Dual (T+I) | D = Dual (A+V) |
Commonly Used Pacemakers
The most often used codes are:
- AAI: the atria are paced, when the intrinsic atrial rhythm falls below the pacemakers threshold
- VVI: the ventricles are paced, when the intrinsic ventricular rhythm falls below the pacemakers threshold
- DDD: the pacemaker records both the atrial and ventricular rate and can pace one of each chambers when needed.
- DDDR: as above, but the pacemaker has a sensor that records a demand for higher cardiac output and can adjust the heart rate accordingly.
- Biventricular pacemakers (CRT-D): leads in both ventricles are present to synchronize contraction. This cardiac synchronization therapy can improve symptoms and survival in some heart failure patients.
- ICD (Internal Cardioversion Device): this device can detect and treat Ventricular Tachycardia and Ventricular Fibrillation. Usually the first treatment is anti-tachy pacing (pacing at a rate +- 10% above the ventricular rate in ventricular tachycardia, which can convert the rhythm to sinus rhythm). If this is not effective an defibrillator shock is delivered, usually with 16-36 Joules of energy. ICDs can save lives in patients who have a high risk of ventricular arrhythmias. All ICDs have optional pacemaker activity to treat bradycardias. New biventricular ICDs have 3 leads: an atrial lead, a left ventricular lead and a right ventricular lead.
Pacemaker Indications
A full list of pacemaker indications can be read in the ESC guidelines on cardiac pacing Vardas. A selection of class I indications are: chronic symptomatic third- or second degree (Mobtiz I or II) atrioventricular block. Syncope with sinus node disease. Alternating bundle branch block. Persisting AV block after surgery.
ICD Indications
Atrial-sensed ventricular-paced rhythm
AV dual-paced rhythm
Pacemaker Malfunction
to be filled in ...
Failure of appropriate capture, atrial
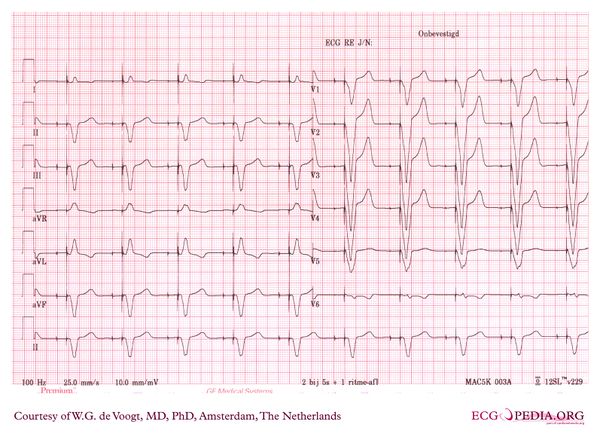
Failure of appropriate capture, ventricular
Failure of appropriate inhibition, atrial
Failure of appropriate inhibition, ventricular
Failure of appropriate pacemaker firing
Retrograde atrial activation
Pacemaker mediated tachycardia
External Links
References
<biblio>
- Vardas pmid=17726042
- Gregoratos pmid=12379588
- Bernstein pmid=11916002
</biblio>