Pathologic Q Waves: Difference between revisions
mNo edit summary |
|||
| (15 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
{{Chapter|Myocardial Infarction}} | |||
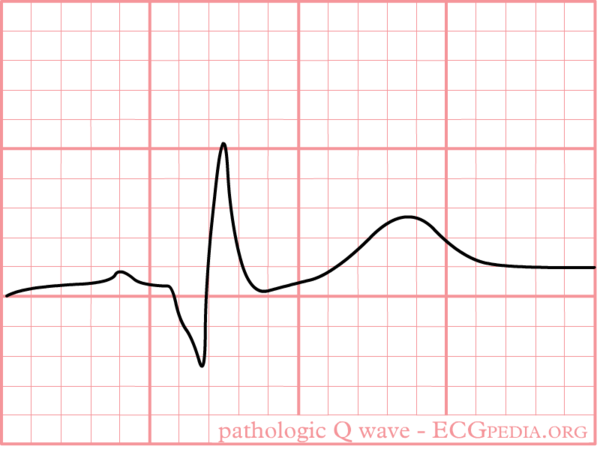
[[Image:PathoQ.png|thumb| A pathologic Q wave]] | [[Image:PathoQ.png|thumb| A pathologic Q wave]] | ||
Pathologic Q waves are a sign of previous [[Myocardial Infarction|myocardial infarction]]. | Pathologic Q waves are a sign of '''previous [[Myocardial Infarction|myocardial infarction]]'''. They are the result of absence of electrical activity. A myocardial infarction can be thought of as an elecrical 'hole' as scar tissue is electrically dead and therefore results in pathologic Q waves. Pathologic Q waves are not an early sign of myocardial infarction, but '''generally take several hours to days to develop'''. Once pathologic Q waves have developed they rarely go away. However, if the myocardial infarction is reperfused early (e.g. as a result of percutaneous coronary intervention) stunned myocardial tissue can recover and pathologic Q waves disappear. In all other situations they '''usually persist indefinitely'''. | ||
The precise criteria for pathologic Q waves have been debated. Here we present the latest definition as accepted by the ESC and ACC.<cite> | The precise criteria for pathologic Q waves have been debated. Here we present the latest definition as accepted by the ESC and ACC.<cite>Thygesen</cite> | ||
;Definition of a pathologic Q wave | ;Definition of a pathologic Q wave | ||
:Any Q wave in leads | :Any Q-wave in leads V2–V3 ≥ 0.02 s or QS complex in leads V2 and V3 | ||
:Q wave > | :Q-wave ≥ 0.03 s and > 0.1 mV deep or QS complex in leads I, II, aVL, aVF, or V4–V6 in any two leads of a contiguous lead grouping (I, aVL,V6; V4–V6; II, III, and aVF) | ||
:R-wave ≥ 0.04 s in V1–V2 and R/S ≥ 1 with a concordant positive T-wave in the absence of a conduction defect | |||
'''Notes''' | '''Notes''' | ||
| Line 13: | Line 15: | ||
For those interested: the [http://www.epi.umn.edu/ecg/mncode.pdf Minnesota Code Classification System for Electrocardiographic Findings] contains a very extensive definition of pathologic Q waves. | For those interested: the [http://www.epi.umn.edu/ecg/mncode.pdf Minnesota Code Classification System for Electrocardiographic Findings] contains a very extensive definition of pathologic Q waves. | ||
The Novacode system further classifies ischemic abnormalities in patients with no known history of myocardial infarction:<cite>novacode</cite> | |||
* High risk of ischemic injury/ Q wave MI: | |||
** Major Q waves: Q >= 50ms or Q >= 40 ms AND R/Q < 4, | |||
* Moderate risk of ischemc injury / possible Q wave MI: | |||
** Q >= 30 ms and ST deviation > 0.20 mV (minor Q waves with STT abnormalities) | |||
** Q >= 40 ms and ST deviation < 0.20mV (moderate Q waves without STT abnormalities) | |||
* Marginal risk of ischemic injury / possible Q wave MI: | |||
** Isolated T wave abnormalities | |||
** Minor Q waves (shallow Q < 30ms) and ST deviation < 0.15 mV | |||
* Low risk of ischemic injury | |||
** No significant Q waves or STT abnormalities | |||
{{clr}} | {{clr}} | ||
== | ==References== | ||
<biblio> | <biblio> | ||
#Alpert pmid=10987628 | #Alpert pmid=10987628 | ||
#Thygesen pmid=17951284 | |||
#novacode pmid=9682893 | |||
</biblio> | </biblio> | ||
Latest revision as of 22:10, 8 January 2012
| This is part of: Myocardial Infarction |
Pathologic Q waves are a sign of previous myocardial infarction. They are the result of absence of electrical activity. A myocardial infarction can be thought of as an elecrical 'hole' as scar tissue is electrically dead and therefore results in pathologic Q waves. Pathologic Q waves are not an early sign of myocardial infarction, but generally take several hours to days to develop. Once pathologic Q waves have developed they rarely go away. However, if the myocardial infarction is reperfused early (e.g. as a result of percutaneous coronary intervention) stunned myocardial tissue can recover and pathologic Q waves disappear. In all other situations they usually persist indefinitely.
The precise criteria for pathologic Q waves have been debated. Here we present the latest definition as accepted by the ESC and ACC.Thygesen
- Definition of a pathologic Q wave
- Any Q-wave in leads V2–V3 ≥ 0.02 s or QS complex in leads V2 and V3
- Q-wave ≥ 0.03 s and > 0.1 mV deep or QS complex in leads I, II, aVL, aVF, or V4–V6 in any two leads of a contiguous lead grouping (I, aVL,V6; V4–V6; II, III, and aVF)
- R-wave ≥ 0.04 s in V1–V2 and R/S ≥ 1 with a concordant positive T-wave in the absence of a conduction defect
Notes
- Absence of pathologic Q waves does not exclude a myocardial infarction!
- Lead III often shows Q waves, which are not pathologic as long as Q waves are absent in leads II and aVF (the contiguous leads)
For those interested: the Minnesota Code Classification System for Electrocardiographic Findings contains a very extensive definition of pathologic Q waves.
The Novacode system further classifies ischemic abnormalities in patients with no known history of myocardial infarction:novacode
- High risk of ischemic injury/ Q wave MI:
- Major Q waves: Q >= 50ms or Q >= 40 ms AND R/Q < 4,
- Moderate risk of ischemc injury / possible Q wave MI:
- Q >= 30 ms and ST deviation > 0.20 mV (minor Q waves with STT abnormalities)
- Q >= 40 ms and ST deviation < 0.20mV (moderate Q waves without STT abnormalities)
- Marginal risk of ischemic injury / possible Q wave MI:
- Isolated T wave abnormalities
- Minor Q waves (shallow Q < 30ms) and ST deviation < 0.15 mV
- Low risk of ischemic injury
- No significant Q waves or STT abnormalities
References
<biblio>
- Alpert pmid=10987628
- Thygesen pmid=17951284
- novacode pmid=9682893
</biblio>