A Narrow QRS Complex Tachycardia Sensitive to Isoptin: Difference between revisions
m (New page: {{NHJ| |mainauthor= '''A.A.M. Wilde, R.H. Bakker''' |edition= 2006,08:268 }} Figure 1|thumb Figure 2|thumb A 54...) |
(No difference)
|
Revision as of 19:10, 8 October 2007
| Author(s) | A.A.M. Wilde, R.H. Bakker | |
| NHJ edition: | 2006,08:268 | |
| These Rhythm Puzzles have been published in the Netherlands Heart Journal and are reproduced here under the prevailing creative commons license with permission from the publisher, Bohn Stafleu Van Loghum. | ||
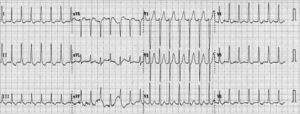
| The ECG can be enlarged twice by clicking on the image and it's first enlargement | ||
A 54-year-old man presented with palpitations. He had no other symptoms. Physical examination revealed, with the exception of a fast regular heart rhythm (200 beats/min), no abnormalities. His ECG is shown in figure 1. Intravenous verapamil terminated the tachycardia and a second ECG (figure 2) was taken.
What is your diagnosis?
Answer Figure 1 shows a narrow-complex tachycardia (rate 180 beats/min). The QRS complex is 84 msec wide, and has an intermediate axis. A P wave is not easy to discern, but could be present in the mid part of the T wave (most clearly seen in leads II and aVF). The Pwave axis cannot be determined. The differential diagnosis of this tachycardia is orthodromic circus movement tachycardia, AV-nodal re-entry tachycardia or atrial tachycardia. The position of the P wave at some distance from the QRS complex is in favour of an orthodromic tachycardia (or an atrial tachycardia with first-degree atrioventricular (AV) block).
Isoptin terminates the tachycardia and that is usually indicative of involvement of the AV node. Hence, an orthodromic tachycardia is the most likely diagnosis. The ECG after termination of the tachycardia (figure 2) showed sinus rhythm with a normal PQ interval (140 msec), followed by a normal QRS complex in the first six beats. In the rhythm strip at the bottom of the panel, the next three QRS complexes are preceded by the same configuration P wave but with a shorter PQ interval (90 msec). These QRS complexes start with a Q wave. In the three precordial leads above the rhythm strip a discrete Δ-wave is visible (electroneutral in V1 and positive in leads V2 and V3). In the left precordial leads (last complex) the Δ-wave changes from positive (V4) to neutral-negative (V6). Hence, this ECG shows evidence of intermittent pre-excitation with a Kent bundle in the inferior wall, presumably just left of the septum. For the exact location of the Kent bundle pre-excitation should be present in the extremity leads.
In conclusion, in the presence of (intermittent) preexcitation the tachycardia is most likely an orthodromic re-entrant tachycardia.