An Old Lady with Chest Pain: Difference between revisions
m (New page: {{NHJ| |mainauthor= '''A.A.M. Wilde''' |edition= 2006:04,154 }} Figure 1|thumb A 90-year-old lady presented with chest pain which had a sudden onset i...) |
(No difference)
|
Revision as of 18:59, 8 October 2007
| Author(s) | A.A.M. Wilde | |
| NHJ edition: | 2006:04,154 | |
| These Rhythm Puzzles have been published in the Netherlands Heart Journal and are reproduced here under the prevailing creative commons license with permission from the publisher, Bohn Stafleu Van Loghum. | ||
| The ECG can be enlarged twice by clicking on the image and it's first enlargement | ||
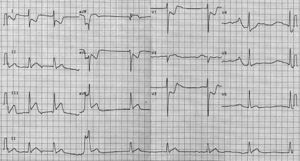
A 90-year-old lady presented with chest pain which had a sudden onset in the middle of the night. There were no other symptoms. She never had experienced similar pain before. There was no other relevant medical history. She was not on any medication. Physical examination revealed no abnormalities. The first ECG is shown in figure 1 (standard calibration).
What is your diagnosis and what would be the next step?
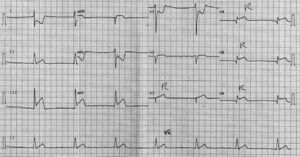
A careful look at the ECG reveals no clear P waves. There is a bradycardic rhythm with initially a slight irregularity in the QRS complexes. In the last part of the ECG, QRS complexes follow each other on a regular basis with 1440 ms intervals (see rhythm strip at the bottom). The QRS width is 120 ms. The ST segments are markedly deviated: ST elevation in lead III and less evident in lead II and aVF and ST depression in leads I, aVL, V1 and V3. In addition there is ST elevation in lead aVR. Based on these ECG changes, the diagnosis should be atrial fibrillation and inferior-posterior myocardial infarction. The slow heart rate suggests the presence of advanced AV-nodal conduction block, a common feature in the setting of inferior wall infarction. ST elevation in lead aVR suggests that the right ventricle is involved as well. A further indication of RV involvement is the rightward displacement of the precordial leads (i.e. the next step should be a rightward pooled ECG; figure 2). This ECG shows clear ST elevation in the right precodial leads and now a regular slow ventricular rhythm, substantiating the diagnosis of advanced AV nodal conduction block (i.e. total AV block in the presence of atrial fibrillation). Acute coronary angiography revealed an (anticipated) proximal right coronary artery occlusion. In both ECGs lead V2 is probably not at the correct position, it is either at the position of V1 (and V1 at the position of V2) or even more displaced to the right.