Should I be worried: Difference between revisions
m (New page: {{NHJ| |mainauthor= '''A.A.M. Wilde, H.L. Tan''' |edition= 2006:01,033 }} Figure 1|thumb A 34-year old man comes to your office. He has read in a newspa...) |
(No difference)
|
Revision as of 17:49, 8 October 2007
| Author(s) | A.A.M. Wilde, H.L. Tan | |
| NHJ edition: | 2006:01,033 | |
| These Rhythm Puzzles have been published in the Netherlands Heart Journal and are reproduced here under the prevailing creative commons license with permission from the publisher, Bohn Stafleu Van Loghum. | ||
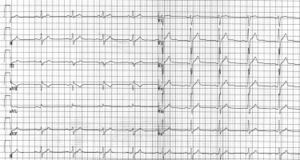
| The ECG can be enlarged twice by clicking on the image and it's first enlargement | ||
A 34-year old man comes to your office. He has read in a newspaper about the familial occurrence of sudden death. He suffered a collapse during an episode of viral meningitis accompanied by high fever a few months earlier. A few years ago his elder brother, who was previously found to have idiopathic atrial fibrillation, died suddenly at the age 32 years. Physical examination reveals no abnormalities, including normal heart sounds. Echocardiographic evaluation reveals no abnormalities either. His baseline ECG is shown in figure 1.
What is your interpretation and what would be or should be your next step(s)?
The ECG shows sinus rhythm of 59 beats/min. Conduction parameters are abnormal; the PQ interval is a little over 200 msec and the QRS width is 120 msec (nonspecific conduction delay). It should be noted that the P-wave morphology is abnormal and that the P-wave duration is at the upper limit of normal as well. The electrical axis is at -30. The ST-T segments are normal in all leads. QT interval is well within normal limits and there is no right precordial ST elevation. The chance that a familiar cardiac disorder is the cause of the sudden death of a young (<40 years of age) close relative is at least 40%.[1] Hence, the presence of an abnormal ECG should alert the physician and specific cardiac abnormalities should be looked for. A familial structural cardiac abnormality seems unlikely because no abnormalities were identified in his deceased brother (idiopathic atrial fibrillation indicates the absence of structural heart disease) nor in your patient. QT prolongation is not present. Delayed conduction in all cardiac compartments should raise the suspicion of an abnormal cardiac sodium channel, i.e. a sodium channelopathy which includes Brugada syndrome, long-QT syndrome type 3 and isolated conduction disease or combinations thereof. Brugada syndrome can be unmasked by placing the right precordial leads one intercostal space (ICS) more cranially (i.e. in the third ICS). In figures 2 and 3 the leads V5 and V6 have been replaced by leads V1 and V2 positioned in the third ICS. A clear type 2 (saddle back) Brugada ECG becomes visible.Wilde The strong suspicion of Brugada syndrome can now be confirmed by a drug challenge. In this case, 100 mg flecainide was infused (for protocol see reference 2) and in addition to significant additional conduction delay at all levels, the right precordial ST segments in the third ICS turn into a coved type (figure 3). Brugada syndrome should be diagnosed and DNA diagnostics should be ordered. In this patient a mutation in the SCN5a gene was identified (G1743E). An electrophysiological study was performed and ventricular fibrillation could reproducibly be induced. An ICD was implanted.
References
- Tan HL, Hofman N, van Langen IM, van der Wal AC, and Wilde AA. Sudden unexplained death: heritability and diagnostic yield of cardiological and genetic examination in surviving relatives. Circulation. 2005 Jul 12;112(2):207-13. DOI:10.1161/CIRCULATIONAHA.104.522581 |
- Wilde AA, Antzelevitch C, Borggrefe M, Brugada J, Brugada R, Brugada P, Corrado D, Hauer RN, Kass RS, Nademanee K, Priori SG, Towbin JA, and Study Group on the Molecular Basis of Arrhythmias of the European Society of Cardiology. Proposed diagnostic criteria for the Brugada syndrome. Eur Heart J. 2002 Nov;23(21):1648-54. DOI:10.1053/euhj.2002.3382 |