MI Diagnosis in LBBB or paced rhythm: Difference between revisions
ST segment depression in the right precordials is actually concordant, not discordant |
mNo edit summary |
||
| (15 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
In case of a [[Intraventricular Conduction|left | [[File:MI_LBBB.png|thumb|Changes in LBBB during ischemia]] | ||
In case of a [[Intraventricular Conduction|left bundle branch block (LBBB)]], infarct diagnosis based on the ECG is difficult. The baseline ST segments and T waves tend to be shifted in a discordant direction with LBBB, which can mask or mimic acute myocardial infarction. However, serial ECGs may show a moving ST segment during ischemia secondary to dynamic supply versus demand characteristics. A new LBBB is always pathological and can be a sign of myocardial infarction. The criteria (Sgarbossa <cite>LBTB</cite>) that can be used in case of a LBBB and suspicion of infarction are: | |||
*ST elevation > 1mm in leads with a positive QRS complex (concordance in ST deviation) (score 5) | *ST elevation > 1mm in leads with a positive QRS complex (concordance in ST deviation) (score 5) | ||
*ST depression > 1 mm in V1-V3 (concordance in ST deviation) (score 3) | *ST depression > 1 mm in V1-V3 (concordance in ST deviation) (score 3) | ||
*ST elevation > 5 mm in leads with a negative QRS complex (inappropriate discordance in ST deviation) (score 2) | *ST elevation > 5 mm in leads with a negative QRS complex (inappropriate discordance in ST deviation) (score 2). This criterion is sensitive, but not specific for ischemia in LBBB. It is however associated with a worse prognosis, when present in LBBB during ischemia.<cite>Wong</cite> | ||
At a score-sum of 3, these criteria have a specificity of 90% for detecting a myocardial infarction. | At a score-sum of 3, these criteria have a specificity of 90% for detecting a myocardial infarction. | ||
During right ventricular pacing the ECG also shows left bundle brach block and the above rules also apply for the diagnosis of myocardial infarction during pacing, however they are less specific.<cite>3</cite><cite>4</cite> In the GUSTO-1 trial the ECG criterion with a high specificity and statistical significance for the diagnosis of an acute MI was:<cite>Gusto</cite> | |||
* ST segment elevation ≥5 mm in leads with a negative QRS complex. | |||
Two other criteria with acceptable specificity were: | |||
*ST elevation ≥1 mm in leads with concordant QRS polarity | |||
*ST depression ≥1 mm in leads V1, V2, or, V3 | |||
{{clr}} | {{clr}} | ||
==Examples== | ==Examples== | ||
<gallery> | <gallery> | ||
Image:MI in LBBB 01.jpg|Acute myocardial infarction in in a patient with a pacemaker and LBBB. Concordant ST elevation in V5-V6 are clearly visible. | Image:MI in LBBB 01.jpg|Case 1: Acute myocardial infarction in in a patient with a pacemaker and LBBB. Concordant ST elevation in V5-V6 are clearly visible. There is discordant ST segment elevation > 5 mm in lead V3. | ||
Image:MI in LBBB 02.jpg|The same patient as in the first example 2 months before the myocardial infarction. Normal LBBB pattern. | Image:MI in LBBB 02.jpg|Case 1: The same patient as in the first example 2 months before the myocardial infarction. Normal LBBB pattern. | ||
Image:LBBB_with_AMI.jpg|Case 2: Acute MI in a patient with LBBB | |||
Image:E000003.jpg|Case 3: Acute MI in a patient with LBBB | |||
Image:E000002.jpg|Case 3: Non-ischemic ECG in this patient | |||
Image:E000406.jpg|Myocardial infarction in a pacemaker patient. The ECG shows LBBB as expected during pacing, however overt repolarization abnormalities are present. | |||
Image:E000405.jpg|Myocardial infarction post primary PCI in a pacemaker patient | |||
Image:V-paced_with_acute_IWMI.png|Ventricular pacemaker with acute inferior infarction | |||
</gallery> | </gallery> | ||
==References== | ==References== | ||
<biblio> | <biblio> | ||
#LBTB pmid= | #LBTB pmid=8559200 | ||
#Wong pmid=15992631 | |||
#3 pmid=18651461 | |||
#4 pmid=15127382 | |||
#Gusto pmid=8602576 | |||
</biblio> | </biblio> | ||
Latest revision as of 09:59, 8 October 2014

In case of a left bundle branch block (LBBB), infarct diagnosis based on the ECG is difficult. The baseline ST segments and T waves tend to be shifted in a discordant direction with LBBB, which can mask or mimic acute myocardial infarction. However, serial ECGs may show a moving ST segment during ischemia secondary to dynamic supply versus demand characteristics. A new LBBB is always pathological and can be a sign of myocardial infarction. The criteria (Sgarbossa LBTB) that can be used in case of a LBBB and suspicion of infarction are:
- ST elevation > 1mm in leads with a positive QRS complex (concordance in ST deviation) (score 5)
- ST depression > 1 mm in V1-V3 (concordance in ST deviation) (score 3)
- ST elevation > 5 mm in leads with a negative QRS complex (inappropriate discordance in ST deviation) (score 2). This criterion is sensitive, but not specific for ischemia in LBBB. It is however associated with a worse prognosis, when present in LBBB during ischemia.Wong
At a score-sum of 3, these criteria have a specificity of 90% for detecting a myocardial infarction.
During right ventricular pacing the ECG also shows left bundle brach block and the above rules also apply for the diagnosis of myocardial infarction during pacing, however they are less specific.34 In the GUSTO-1 trial the ECG criterion with a high specificity and statistical significance for the diagnosis of an acute MI was:Gusto
- ST segment elevation ≥5 mm in leads with a negative QRS complex.
Two other criteria with acceptable specificity were:
- ST elevation ≥1 mm in leads with concordant QRS polarity
- ST depression ≥1 mm in leads V1, V2, or, V3
Examples
-
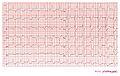
Case 1: Acute myocardial infarction in in a patient with a pacemaker and LBBB. Concordant ST elevation in V5-V6 are clearly visible. There is discordant ST segment elevation > 5 mm in lead V3.
-
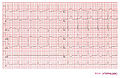
Case 1: The same patient as in the first example 2 months before the myocardial infarction. Normal LBBB pattern.
-
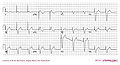
Case 2: Acute MI in a patient with LBBB
-
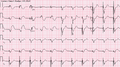
Case 3: Acute MI in a patient with LBBB
-
Case 3: Non-ischemic ECG in this patient
-
Myocardial infarction in a pacemaker patient. The ECG shows LBBB as expected during pacing, however overt repolarization abnormalities are present.
-
Myocardial infarction post primary PCI in a pacemaker patient
-
Ventricular pacemaker with acute inferior infarction
References
<biblio>
- LBTB pmid=8559200
- Wong pmid=15992631
- 3 pmid=18651461
- 4 pmid=15127382
- Gusto pmid=8602576
</biblio>