Myocardial Infarction: Difference between revisions
No edit summary |
|||
| (39 intermediate revisions by 16 users not shown) | |||
| Line 1: | Line 1: | ||
<div style="float:left">__TOC__</div> | |||
{{authors| | {{authors| | ||
|mainauthor= [[user:Vdbilt|I.A.C. van der Bilt, MD]] | |mainauthor= [[user:Vdbilt|I.A.C. van der Bilt, MD]] | ||
| Line 4: | Line 5: | ||
|supervisor= | |supervisor= | ||
}} | }} | ||
Ischemia occurs when part of the | {{clr}} | ||
{{box| | |||
Ischemia occurs when part of the heart muscle, the myocardium, is deprived of oxygen and nutrients. | |||
Common causes of ischemia are: | Common causes of ischemia are: | ||
* Narrowing or obstruction of a coronary artery. | * Narrowing or obstruction of a coronary artery. | ||
* A rapid arrhythmia, causing | * A rapid arrhythmia, causing an imbalance in supply and demand for energy. | ||
A short period of ischemia causes '' | A short period of ischemia causes ''reversible'' effects: The heart cells will be able to recover. When the episode of ischemia lasts for a longer period of time, heart muscle cells die. This is called a '''heart attack''' or '''myocardial infarction'''. That is why it is critical to recognize ischemia on the ECG in an early stage. | ||
Severe ischemia | Severe ischemia results in ECG changes within minutes. While the ischemia lasts, several ECG changes will occur and disappear again. Therefore, it may be difficult to estimate the duration of the ischemia on the ECG, which is crucial for adequate treatment. | ||
'''Signs and symptoms of myocardial ischemia:''' | '''Signs and symptoms of myocardial ischemia:''' | ||
| Line 18: | Line 21: | ||
* Nausea | * Nausea | ||
* Shock (manifesting as paleness, low blood pressure, fast weak pulse) shock | * Shock (manifesting as paleness, low blood pressure, fast weak pulse) shock | ||
* Rhythm | * Rhythm disturbances (in particular, increasing prevalence of ventricular ectopia, ventricular tachycardia, AV block) | ||
}} | |||
===Risk assessment of | {{clr}} | ||
===Risk assessment of Cardiovascular disease=== | |||
*Male | Narrowing of the coronary artery, leading to a myocardial infarction, usually develops over several years. An increased risk of cardiovascular disease, which may lead to a myocardial infarction or cerebrovascular accident, can be estimated using [http://www.escardio.org/communities/EACPR/toolbox/health-professionals/Pages/SCORE-Risk-Charts.aspx SCORE system] which is developed by the European Society of cardiology (ESC). | ||
As shown in the figure, the most important risk factors for myocardial infarction are: | |||
*Male sex | |||
*Smoking | *Smoking | ||
*Hypertension | *Hypertension | ||
| Line 28: | Line 33: | ||
*Hypercholesterolemia | *Hypercholesterolemia | ||
An [[Exercise Testing|exercise test]] such as a bicycle or | ===Risk assessment of ischemia=== | ||
An [[Exercise Testing|exercise test]] such as a bicycle or treadmill test, may be useful in detecting myocardial ischemia after exercise.<cite>accexercise</cite> In such a test, continuous ECG monitoring is performed during exercise. The ST-segment, blood pressure and clinical status of the patient (i.e. chest complaints) are monitored during and after the test. | |||
An [[Exercise Testing|exercise test]] is positive for myocardial ischemia when the following criteria are met: | An [[Exercise Testing|exercise test]] is positive for myocardial ischemia when the following criteria are met: | ||
* Horizontal or downsloping ST-depression of > 1mm, 60 or 80ms after the J-point | * Horizontal or downsloping ST-depression of >1mm, 60 or 80ms after the J-point | ||
* ST elevation of > 1.0 mm | * ST elevation of > 1.0 mm | ||
{{clr}} | {{clr}} | ||
==Diagnosis of myocardial infarction== | ==Diagnosis of myocardial infarction== | ||
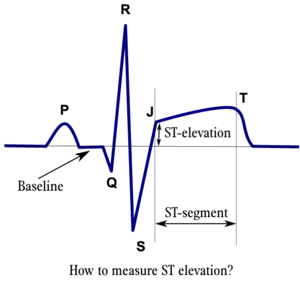
[[Image:Stelevatie_en.png|thumb|ST elevation is measured | [[Image:Stelevatie_en.png|thumb|300px|ST elevation is measured at the junctional or J-point]] | ||
The diagnosis of acute myocardial infarction is not only based on the ECG. A myocardial is defined as:<cite>Alpert</cite> | The diagnosis of acute myocardial infarction is not only based on the ECG. A myocardial infarction is defined as:<cite>Alpert</cite> | ||
* Elevated blood levels of cardiac enzymes ([[w:Creatine_kinase|CKMB]] or [[w:Troponin|Troponin T]]) AND | * Elevated blood levels of cardiac enzymes ([[w:Creatine_kinase|CKMB]] or [[w:Troponin|Troponin T]]) AND | ||
* One of the following criteria are met: | * One of the following criteria are met: | ||
** The patient has typical complaints | ** The patient has typical complaints, | ||
** The ECG shows ST elevation or depression | ** The ECG shows ST elevation or depression. | ||
** [[Pathologic_Q_Waves|pathological Q waves]] develop on the ECG | ** [[Pathologic_Q_Waves|pathological Q waves]] develop on the ECG | ||
** A coronary intervention had been performed (such as stent placement) | ** A coronary intervention had been performed (such as stent placement) | ||
So detection of elevated serum | So detection of elevated serum cardiac enzymes is more important than ECG changes. However, the cardiac enzymes can only be detected in the serum 5-7 hours after the onset of the myocardial infarction. So, especially in the first few hours after the myocardial infarction, the ECG can be crucial. | ||
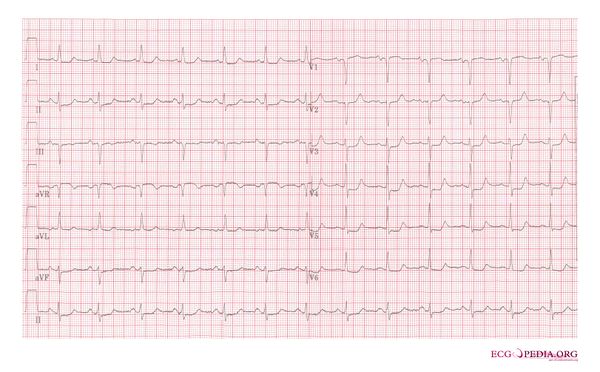
ECG Manifestations of Acute Myocardial Ischaemia (in Absence of LVH and [[MI Diagnosis in LBBB|LBBB]])are <cite>Thygesen</cite>: | |||
;ST elevation | |||
:New ST elevation at the J-point in two contiguous leads with the cut-off points: ≥0.2 mV in men or ≥ 0.15 mV in women in leads V2–V3 and/or ≥ 0.1 mV in other leads. | |||
;ST depression and T-wave changes. | |||
:New horizontal or down-sloping ST depression >0.05 mV in two contiguous leads; and/or T inversion ≥0.1 mVin two contiguous leads with prominent R-wave or R/S ratio ≥ 1 | |||
A study using MRI to diagnose myocardial infarction has shown that more emphasis on ST segment depression could greatly improve the yield of the ECG in the diagnosis of myocardial infarction (sensitivity increase from 50% to 84%).<cite>martin</cite> | |||
Myocardial infarction diagnosis in left or right bundle branch block can be difficult, but is explained in these seperate chapters: | Myocardial infarction diagnosis in left or right bundle branch block can be difficult, but it is explained in these seperate chapters: | ||
*[[MI Diagnosis in LBBB]] | *[[MI Diagnosis in LBBB|MI diagnosis in left bundle branch block or paced rhytm]] | ||
*[[MI Diagnosis in RBBB]] | *[[MI Diagnosis in RBBB]] | ||
{{clr}} | {{clr}} | ||
==The location of the infarct== | ==The location of the infarct== | ||
<div style="float:right;margin-left:10px"> | |||
<gallery perRow="2"> | |||
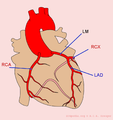
Image:coronary_anatomy.png| An overview of the coronary arteries. LM = 'Left Main' = mainstem; LAD = 'Left Anterior Descending' artery; RCX = Ramus Circumflexus; RCA = 'Right Coronary Artery'. | |||
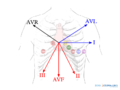
Image:lead_overview.png|Overview of the separate ECG leads. The lead with ST segment elevation 'highlights' the infarct. An infarction of the inferior wall will result in ST segment elevation in leads II, III and AVF. A lateral wall infarct results in ST segment elevation in leads I and AVL. An Anterior wall infarct results in ST segment elevation in the precordial leads. | |||
Image:MI_colours_en.png|The coloured figure shows contiguous leads in matching colors | |||
Image:MIregions.jpg|The ST segment elevation points at the infarct location. Inferior MI=ST segment elevation in red regions (lead II,III and AVF). Lateral MI = ST elevation in blue leads (lead I, AVL, V5-V6). Anterio MI: ST segment elevation in yellow region (V1-V4). Left main stenosis: ST elevation in gray area (AVR) | |||
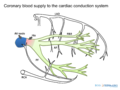
Image:conduction_blood_supply.png|The coronary blockade can cause conduction block, on AV nodal, His or bundle branch level. | |||
</gallery> | |||
</div> | |||
The heartmuscle itself is very limited in its capacity to extract oxygen in the blood that is being pumped. Only the inner layers (the endocardium) profit from this oxygenrich blood. The outer layers of the heart (the epicardium) are dependent on the coronary arteries for the supply of oxygen and nutrients. With aid of an ECG, the occluded coronary can be identified. This is valuable information for the clinician, because treatment and complications of for instance an '''anterior wall infarction''' is different than those of an '''inferior wall infarction'''. The anterior wall performs the main pump function, and decay of the function of this wall will lead to decrease of bloodpressure, increase of heartrate, shock and on a longer term: heart failure. An inferior wall infarction is often accompanied with a decrease in heartrate because of involvement of the sinusnode. Longterm effects of an inferior wall infarction are usually less severe than those of an anterior wall infarction. | The heartmuscle itself is very limited in its capacity to extract oxygen in the blood that is being pumped. Only the inner layers (the endocardium) profit from this oxygenrich blood. The outer layers of the heart (the epicardium) are dependent on the coronary arteries for the supply of oxygen and nutrients. With aid of an ECG, the occluded coronary can be identified. This is valuable information for the clinician, because treatment and complications of for instance an '''anterior wall infarction''' is different than those of an '''inferior wall infarction'''. The anterior wall performs the main pump function, and decay of the function of this wall will lead to decrease of bloodpressure, increase of heartrate, shock and on a longer term: heart failure. An inferior wall infarction is often accompanied with a decrease in heartrate because of involvement of the sinusnode. Longterm effects of an inferior wall infarction are usually less severe than those of an anterior wall infarction. | ||
The heart is supplied of oxygen and nutrients by the right and left coronary arteries. The left | The heart is supplied of oxygen and nutrients by the right and left coronary arteries. The left coronary artery (the '''Left Main''' or LM) divides itself in the '''left anterior descending''' artery (LAD) and the '''ramus circumflexus''' (RCX). The '''right coronary artery''' (RCA) connects to the '''ramus descendens posterior '''(RDP). With 20% of the normal population the RDP is supplied by the RCX. This called '''left dominance'''. | ||
Below you can find several different types of myocardial infarcation. Click on the specific infarct location to see examples. | Below you can find several different types of myocardial infarcation. Click on the specific infarct location to see examples. | ||
| Line 76: | Line 92: | ||
!localisation | !localisation | ||
!ST elevation | !ST elevation | ||
! | !Reciprocal ST depression | ||
!coronary artery | !coronary artery | ||
|- | |- | ||
| Line 87: | Line 103: | ||
| V1-V4, disappearance of septum Q in leads V5,V6 | | V1-V4, disappearance of septum Q in leads V5,V6 | ||
| none | | none | ||
| LAD | | LAD-septal branches | ||
|- | |- | ||
| [[Lateral MI]] | | [[Lateral MI]] | ||
| I, aVL, V5, V6 | | I, aVL, V5, V6 | ||
| II,III, aVF | | II,III, aVF | ||
| | | LCX or MO | ||
|- | |- | ||
| [[Inferior MI]] | | [[Inferior MI]] | ||
| Line 115: | Line 131: | ||
|- | |- | ||
|} | |} | ||
The localisation of the occlusion can be adequately visualized using a coronary angiogram (CAG). On the CAG report, the place of the occlusion is often graded with a number (for example LAD(7)) using the classification of the American Heart Association.<cite>AHACAG</cite> | The localisation of the occlusion can be adequately visualized using a coronary angiogram (CAG). On the CAG report, the place of the occlusion is often graded with a number (for example LAD(7)) using the classification of the American Heart Association.<cite>AHACAG</cite> | ||
{{clr}} | |||
==Development of the ECG during persistent ischemia== | ==Development of the ECG during persistent ischemia== | ||
[[Image:AMI_evolutie.png|thumb| The evolution of an infarct on the ECG. ST elevation, Q wave formation, T wave inversion, normalisation with a persistent Q wave]] | [[Image:AMI_evolutie.png|thumb| The evolution of an infarct on the ECG. ST elevation, Q wave formation, T wave inversion, normalisation with a persistent Q wave]] | ||
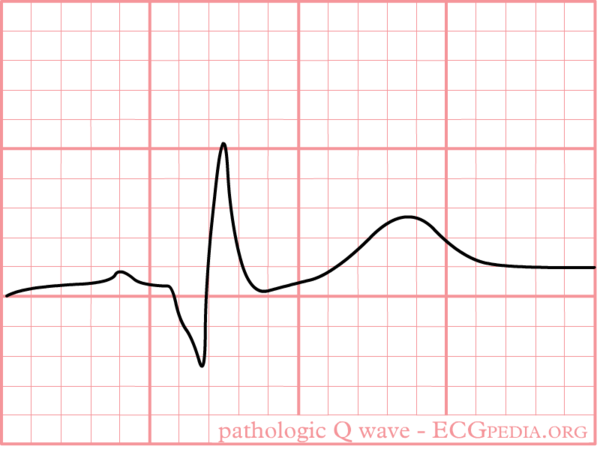
[[Image:PathoQ.png|thumb| A [[Pathologic_Q_Waves|pathological Q wave]]]] | [[Image:PathoQ.png|thumb| A [[Pathologic_Q_Waves|pathological Q wave]]]] | ||
[[File:DVA1995.jpg|thumb|Wellens syndrome: symmetrical negative T wave in pre-cordial leads without R loss of R waves can regularly be observed in early anterior ischemia. Many patients with Wellens syndrome / sign turn out to have a critical proximal LAD stenosis<cite>WellensSign</cite>.]] | |||
[[Image:anteriorMInegativeT.png|thumb| Typical negative T waves post anterior myocardial infarction. This patient also shows QTc prolongation. Whether this has an effect on prognosis is debated.<cite>Novotny</cite><cite>Jensen</cite><cite>Chevalier</cite>]] | |||
The cardiomyocytes in the ''subendocardial'' layers are especcially vulnerable for a decreased perfusion. Subendocardial ischemia manifests as ST depression and is usually reversible. In a myocardial infarction ''transmural ischemia'' develops. | The cardiomyocytes in the ''subendocardial'' layers are especcially vulnerable for a decreased perfusion. Subendocardial ischemia manifests as ST depression and is usually reversible. In a myocardial infarction ''transmural ischemia'' develops. | ||
In the first hours and days after the onset of a myocardial infarction, several changes can be observed on the ECG. First, '''large peaked T waves''' (or ''hyperacute'' T waves), then '''ST elevation''', then'''negative T waves''' and finally '''[[Pathologic_Q_Waves|pathologic Q waves]]''' develop. | In the first hours and days after the onset of a myocardial infarction, several changes can be observed on the ECG. First, '''large peaked T waves''' (or ''hyperacute'' T waves), then '''ST elevation''', then '''negative T waves''' and finally '''[[Pathologic_Q_Waves|pathologic Q waves]]''' develop. | ||
'''Wellens syndrome''' or sign (see image) can be an early ECG warning sign of critical anterior ischemia before the development of overt mocardial infarction. | |||
{| class="wikitable" | {| class="wikitable" | ||
| Line 130: | Line 150: | ||
|+'''Evolution of the ECG during a myocardial infarct''' | |+'''Evolution of the ECG during a myocardial infarct''' | ||
|- | |- | ||
! | !Time from onset of symptoms | ||
! | !ECG | ||
! | !Changes in the heart | ||
|- | |- | ||
!minutes | !minutes | ||
| hyperacute T waves (tall T waves), ST-elevation | |||
| reversible ischemic damage | |||
| hyperacute T waves ( | |||
ST-elevation | |||
|- | |- | ||
!hours | !hours | ||
| ST-elevation, with terminal negative T waves, negative T waves (these can last for days to months) | |||
| onset of myocardial necrosis [[Image:Heart_ant_wall_infarction.jpg|left|150px|Thumb|An acute anterior myocardial infarction typically shows ST elevation on the ECG]] | |||
| ST-elevation, with terminal negative T | |||
negative T | |||
|- | |- | ||
!days | !days | ||
| | | [[Pathologic Q Waves]] | ||
| [[ | | scar formation [[Image:Heart_ant_wall_scar_sa.jpg|left|150px|Thumb|A transmural anterior myocardial infarction with scar formation and [[Pathologic Q Waves]]]] | ||
|- | |- | ||
|} | |} | ||
{{clr}} | {{clr}} | ||
==Subendendocardial Ischemia== | |||
[[File:Subendocardial_ischemia2.jpg|thumb|An example of subendocardial ischemia with diffuse ST depression]] | |||
Subendocardial ischemia is ischemia that is not transmural. It is mostly caused by demand ischemia where energy supply to cardiomyocytes is insufficient for the work force, e.g. during extreme hypertension, aortic valve stenosis, extreme left ventricular hypertension, anemia, atrial fibrillation with rapid ventricular response. | |||
On the ECG often diffuse ST depression is present. Cardiac enzymes (CK-MB, Troponine) may or may not be elevated depending on the severity. | |||
{{box| | |||
==References== | ==References== | ||
<biblio> | <biblio> | ||
#Wung pmid=16777513 | #Wung pmid=16777513 | ||
#martin pmid=17825710 | |||
#Alpert pmid=10987628 | #Alpert pmid=10987628 | ||
#accexercise pmid=12356646 | #accexercise pmid=12356646 | ||
| Line 162: | Line 183: | ||
#LBTB pmid=11265742 | #LBTB pmid=11265742 | ||
#AHACAG pmid=1116248 | #AHACAG pmid=1116248 | ||
#Novotny pmid=18019666 | |||
#Chevalier pmid=12716101 | |||
#Jensen pmid=15851335 | |||
#Thygesen pmid=17951284 | |||
#Wong pmid=15992631 | |||
#WellensSign pmid=6121481 | |||
</biblio> | </biblio> | ||
}} | |||
{{box| | |||
==External Links== | |||
A good introduction to [[http://www.askdrwiki.com/mediawiki/index.php?title=Coronary_Angiography coronary angiography]] | |||
}} | |||
[[Category:ECG Textbook]] | |||
Latest revision as of 21:53, 28 October 2012
| Author(s) | I.A.C. van der Bilt, MD | |
| Moderator | I.A.C. van der Bilt, MD | |
| Supervisor | ||
| some notes about authorship | ||
Ischemia occurs when part of the heart muscle, the myocardium, is deprived of oxygen and nutrients. Common causes of ischemia are:
- Narrowing or obstruction of a coronary artery.
- A rapid arrhythmia, causing an imbalance in supply and demand for energy.
A short period of ischemia causes reversible effects: The heart cells will be able to recover. When the episode of ischemia lasts for a longer period of time, heart muscle cells die. This is called a heart attack or myocardial infarction. That is why it is critical to recognize ischemia on the ECG in an early stage.
Severe ischemia results in ECG changes within minutes. While the ischemia lasts, several ECG changes will occur and disappear again. Therefore, it may be difficult to estimate the duration of the ischemia on the ECG, which is crucial for adequate treatment.
Signs and symptoms of myocardial ischemia:
- Crushing pain on the chest (angina pectoris), behind the sternum, often radiating to the lower jaw or the left arm
- Fear of dying
- Nausea
- Shock (manifesting as paleness, low blood pressure, fast weak pulse) shock
- Rhythm disturbances (in particular, increasing prevalence of ventricular ectopia, ventricular tachycardia, AV block)
Risk assessment of Cardiovascular disease
Narrowing of the coronary artery, leading to a myocardial infarction, usually develops over several years. An increased risk of cardiovascular disease, which may lead to a myocardial infarction or cerebrovascular accident, can be estimated using SCORE system which is developed by the European Society of cardiology (ESC). As shown in the figure, the most important risk factors for myocardial infarction are:
- Male sex
- Smoking
- Hypertension
- Diabetes Mellitus
- Hypercholesterolemia
Risk assessment of ischemia
An exercise test such as a bicycle or treadmill test, may be useful in detecting myocardial ischemia after exercise.accexercise In such a test, continuous ECG monitoring is performed during exercise. The ST-segment, blood pressure and clinical status of the patient (i.e. chest complaints) are monitored during and after the test.
An exercise test is positive for myocardial ischemia when the following criteria are met:
- Horizontal or downsloping ST-depression of >1mm, 60 or 80ms after the J-point
- ST elevation of > 1.0 mm
Diagnosis of myocardial infarction
The diagnosis of acute myocardial infarction is not only based on the ECG. A myocardial infarction is defined as:Alpert
- Elevated blood levels of cardiac enzymes (CKMB or Troponin T) AND
- One of the following criteria are met:
- The patient has typical complaints,
- The ECG shows ST elevation or depression.
- pathological Q waves develop on the ECG
- A coronary intervention had been performed (such as stent placement)
So detection of elevated serum cardiac enzymes is more important than ECG changes. However, the cardiac enzymes can only be detected in the serum 5-7 hours after the onset of the myocardial infarction. So, especially in the first few hours after the myocardial infarction, the ECG can be crucial.
ECG Manifestations of Acute Myocardial Ischaemia (in Absence of LVH and LBBB)are Thygesen:
- ST elevation
- New ST elevation at the J-point in two contiguous leads with the cut-off points: ≥0.2 mV in men or ≥ 0.15 mV in women in leads V2–V3 and/or ≥ 0.1 mV in other leads.
- ST depression and T-wave changes.
- New horizontal or down-sloping ST depression >0.05 mV in two contiguous leads; and/or T inversion ≥0.1 mVin two contiguous leads with prominent R-wave or R/S ratio ≥ 1
A study using MRI to diagnose myocardial infarction has shown that more emphasis on ST segment depression could greatly improve the yield of the ECG in the diagnosis of myocardial infarction (sensitivity increase from 50% to 84%).martin
Myocardial infarction diagnosis in left or right bundle branch block can be difficult, but it is explained in these seperate chapters:
The location of the infarct
-
An overview of the coronary arteries. LM = 'Left Main' = mainstem; LAD = 'Left Anterior Descending' artery; RCX = Ramus Circumflexus; RCA = 'Right Coronary Artery'.
-
Overview of the separate ECG leads. The lead with ST segment elevation 'highlights' the infarct. An infarction of the inferior wall will result in ST segment elevation in leads II, III and AVF. A lateral wall infarct results in ST segment elevation in leads I and AVL. An Anterior wall infarct results in ST segment elevation in the precordial leads.
-
The coloured figure shows contiguous leads in matching colors
-
The ST segment elevation points at the infarct location. Inferior MI=ST segment elevation in red regions (lead II,III and AVF). Lateral MI = ST elevation in blue leads (lead I, AVL, V5-V6). Anterio MI: ST segment elevation in yellow region (V1-V4). Left main stenosis: ST elevation in gray area (AVR)
-
The coronary blockade can cause conduction block, on AV nodal, His or bundle branch level.
The heartmuscle itself is very limited in its capacity to extract oxygen in the blood that is being pumped. Only the inner layers (the endocardium) profit from this oxygenrich blood. The outer layers of the heart (the epicardium) are dependent on the coronary arteries for the supply of oxygen and nutrients. With aid of an ECG, the occluded coronary can be identified. This is valuable information for the clinician, because treatment and complications of for instance an anterior wall infarction is different than those of an inferior wall infarction. The anterior wall performs the main pump function, and decay of the function of this wall will lead to decrease of bloodpressure, increase of heartrate, shock and on a longer term: heart failure. An inferior wall infarction is often accompanied with a decrease in heartrate because of involvement of the sinusnode. Longterm effects of an inferior wall infarction are usually less severe than those of an anterior wall infarction.
The heart is supplied of oxygen and nutrients by the right and left coronary arteries. The left coronary artery (the Left Main or LM) divides itself in the left anterior descending artery (LAD) and the ramus circumflexus (RCX). The right coronary artery (RCA) connects to the ramus descendens posterior (RDP). With 20% of the normal population the RDP is supplied by the RCX. This called left dominance.
Below you can find several different types of myocardial infarcation. Click on the specific infarct location to see examples.
| localisation | ST elevation | Reciprocal ST depression | coronary artery |
|---|---|---|---|
| Anterior MI | V1-V6 | None | LAD |
| Septal MI | V1-V4, disappearance of septum Q in leads V5,V6 | none | LAD-septal branches |
| Lateral MI | I, aVL, V5, V6 | II,III, aVF | LCX or MO |
| Inferior MI | II, III, aVF | I, aVL | RCA (80%) or RCX (20%) |
| Posterior MI | V7, V8, V9 | high R in V1-V3 with ST depression V1-V3 > 2mm (mirror view) | RCX |
| Right Ventricle MI | V1, V4R | I, aVL | RCA |
| Atrial MI | PTa in I,V5,V6 | PTa in I,II, or III | RCA |
The localisation of the occlusion can be adequately visualized using a coronary angiogram (CAG). On the CAG report, the place of the occlusion is often graded with a number (for example LAD(7)) using the classification of the American Heart Association.AHACAG
Development of the ECG during persistent ischemia



The cardiomyocytes in the subendocardial layers are especcially vulnerable for a decreased perfusion. Subendocardial ischemia manifests as ST depression and is usually reversible. In a myocardial infarction transmural ischemia develops.
In the first hours and days after the onset of a myocardial infarction, several changes can be observed on the ECG. First, large peaked T waves (or hyperacute T waves), then ST elevation, then negative T waves and finally pathologic Q waves develop.
Wellens syndrome or sign (see image) can be an early ECG warning sign of critical anterior ischemia before the development of overt mocardial infarction.
| Time from onset of symptoms | ECG | Changes in the heart |
|---|---|---|
| minutes | hyperacute T waves (tall T waves), ST-elevation | reversible ischemic damage |
| hours | ST-elevation, with terminal negative T waves, negative T waves (these can last for days to months) | onset of myocardial necrosis  |
| days | Pathologic Q Waves | scar formation  |
Subendendocardial Ischemia
Subendocardial ischemia is ischemia that is not transmural. It is mostly caused by demand ischemia where energy supply to cardiomyocytes is insufficient for the work force, e.g. during extreme hypertension, aortic valve stenosis, extreme left ventricular hypertension, anemia, atrial fibrillation with rapid ventricular response. On the ECG often diffuse ST depression is present. Cardiac enzymes (CK-MB, Troponine) may or may not be elevated depending on the severity.
{{{1}}}
External Links
A good introduction to [coronary angiography]