|
|
| (One intermediate revision by the same user not shown) |
| Line 11: |
Line 11: |
|
| |
|
| [[Puzzle 2005_2_67|Answer]] | | [[Puzzle 2005_2_67|Answer]] |
|
| |
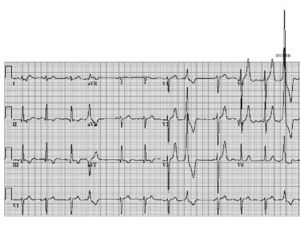
| [[Image:Puzzle_2005_2_67_fig2.jpg|Figure 1|thumb]]
| |
| Any patient with an old myocardial infarction, reduced
| |
| ejection fraction and occasional palpitations with
| |
| dizziness needs serious attention. The patient is at risk
| |
| for sudden cardiac death and ICD therapy has been
| |
| proposed (the MADIT-II and SCD-Heft studies).
| |
| Holter monitoring should be considered mandatory in
| |
| the work-up. The presence of nonsustained ventricular
| |
| tachycardia, a possible explanation for the symptoms,
| |
| identifies an even higher-risk patient (±30% mortality
| |
| in two years in inducible patients during electrophysiological
| |
| study; MADIT II study).
| |
| The extrasystoles have a right bundle branch block
| |
| morphology indicating an origin from the left ventricle.
| |
| The exact site of origin should be derived from the
| |
| information that comes from the extremity leads. There
| |
| is one extrasystole in the extremity leads exactly at the
| |
| moment that the leads change. Hence it should first be
| |
| decided whether the extra is recorded in leads I, II and
| |
| III or in aVR, aVL and aVF.
| |
| The clue is in the morphology of the extra in these leads.
| |
| A ventricular extrasystole can not be completely positive
| |
| in lead II and completely negative in lead III. The two
| |
| leads are 60° apart and concordantly the morphology
| |
| of the complexes in these leads is usually somewhat
| |
| similar. An opposite complex in aVL and aVF is well
| |
| possible and indicates an origin in the inferior wall. In
| |
| that case, the morphology of the ectopy in II and III
| |
| would also be expected to be negative. Indeed, this was
| |
| the case as shown in figure 2, which is the same ECG
| |
| printed in a different format.
| |
| Hence, the origin of the extras is in the inferior wall
| |
| and thus in the area of the old myocardial infarction. The
| |
| patient needs a serious work-up and an ICD should at
| |
| least be considered (MADIT II, SCD-Heft). In the
| |
| presence of nonsustained VTs on Holter monitoring
| |
| (and inducibility during EPS) a class I indication for
| |
| ICD implantation (according to the NVVC guidelines)
| |
| is established.
| |
| Author(s) |
A.A.M. Wilde, R.B.A. van den Brink
|
| NHJ edition: |
2005:2,67
|
| These Rhythm Puzzles have been published in the Netherlands Heart Journal and are reproduced here under the prevailing creative commons license with permission from the publisher, Bohn Stafleu Van Loghum. |
|
| The ECG can be enlarged twice by clicking on the image and it's first enlargement
|
A 64-year-old man had an inferior myocardial infarction ten years ago. Lately he has been having palpitations with occasional dizziness. He sought the attention of his cardiologist. Physical examination revealed no particular abnormalities with the exception
of a laterally displaced ictus cordis. His 12-lead ECG, shown in figure 1, was in sinus rhythm with some extrasystoles. The electrical axis is vertical and the Q waves and abnormal ST-T segments in the inferior leads are compatible with an old inferior myocardial infarction. An echocardiogram revealed reduced left ventricular function with extended inferior wall
akinesia. The left ventricular ejection fraction was estimated to be 30%.
The questions to address are: what is the meaning of the extrasystoles, where do they come from and should further investigations be performed?
Answer