Approach to the Wide Complex Tachycardia: Difference between revisions
No edit summary |
|||
| Line 3: | Line 3: | ||
* Younger patient with known paroxysmal tachycardias and who is hemodynamically stable = most like SVT | * Younger patient with known paroxysmal tachycardias and who is hemodynamically stable = most like SVT | ||
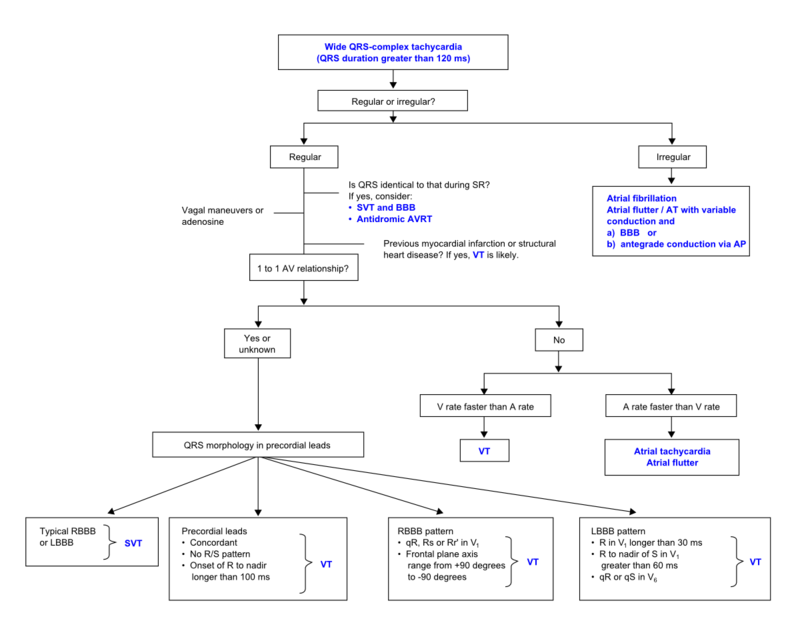
== The ACC algorithm <cite>ACC</cite>== | == The ACC algorithm <cite>ACC</cite>== | ||
[[File: | [[File:VT_algorythm_en.png|800px|thumb|left|SVT vs VT algorhytm. Adapted from <cite>ACC</cite>]] | ||
{{clr}} | {{clr}} | ||
Revision as of 19:03, 28 March 2010
During wide complex tachycardia (heart rate > 100/min, QRS > 0.12 sec) the differentiation between supraventricular and ventricular origin of the arrhythmia is important to guide therapy. Several algorithms have been developed to aid in this differentiation (below). It is important to keep in mind that a good estimate of VT versus SVT can be made based on the clinical vignette:
- 'Horizontal entrance' into the ER. Older patient with previous myocardial infarction = most likely VT
- Younger patient with known paroxysmal tachycardias and who is hemodynamically stable = most like SVT
The ACC algorithm [1]
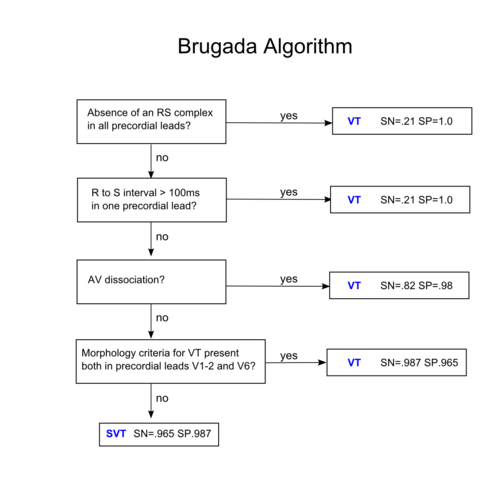
Brugada criteria
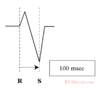
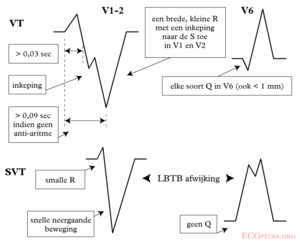
| Morphological criteria (if the above criteria are inconclusive) | ||
|---|---|---|
| LBBB pattern | ||
| Initial R more than 40ms? | Yes => VT | |
| Slurred or notched downwards leg of S wave in leads V1 or V2 | Yes => VT | |
| Beginning of Q to nadir QS >60 ms in V1 or V2? | Yes => VT | LR >50:1 |
| Q or QS in V6? | Yes => VT | LR >50:1 |
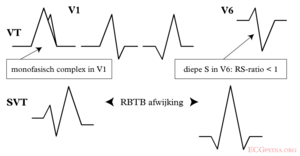
| RBBB pattern | ||
| Monofasic R or qR in V1? | Yes => VT | |
| R taller than R' (rabbit-ear sign)? | Yes => VT | LR >50:1 |
| rS in V6? | Yes => VT | LR >50:1 |
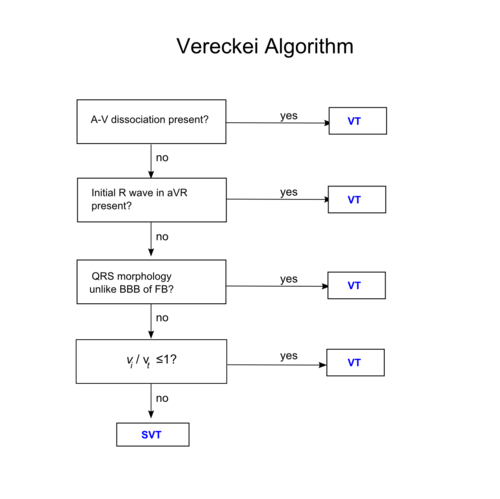
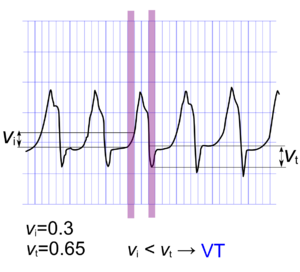
Vereckei algorithm [2]
Examples
Wide complex tachycardia. No AV dissociation. RBBB. Resembles sinus rhythm from the same patient. Conclusion: SVT with RBBB
Wide complex tachycardia. LBBB configuration. Absence of RS in the chest leads. AV dissociation is present. Conclusion: VT
Wide complex tachycardia. LBBB configuration. Absence of RS in the chest leads. AV dissociation is present. Conclusion: VT
Referenties
Error fetching PMID 2022022:
Error fetching PMID 17272358:
- Error fetching PMID 14563598:
- Error fetching PMID 17272358:
- Error fetching PMID 2022022: