Arrhythmogenic Right Ventricular Cardiomyopathy
| Author(s) | J.S.S.G. de Jong, MD | |
| Moderator | J.S.S.G. de Jong, MD | |
| Supervisor | ||
| some notes about authorship | ||
Arrhythmogenic Right Ventricular Cardiomyopathy, (ARVC, or ARVD: Arrhythmogenic Right Ventricular Disease) is characterized by fatty replacement and fibrosis of the heart. Most commonly the right ventricle apex and outflow tract are involved. However the left ventricle can be affected to.[2]
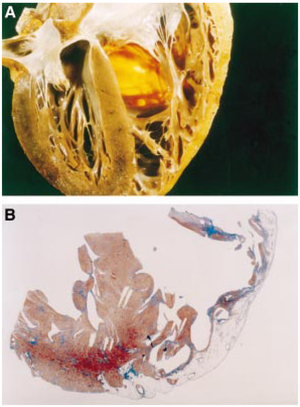
As a result of the fatty replacement and fibrosis, ventricular arrhythmias are common in this disease and can lead to palpitations, syncope and sudden death. At more advanced ages right ventricular pump failure can occur.
The diagnosis is based on major and minor criteria, as published by the European Society of Cardiology.[3]
ARVC is a progressive disease. The incidence is estimated to be 1:3.000-1:10.000. Manifestations are usually seen in teenagers. Although the diagnosis is more often made in athletes, sports are not thought to have a causative relationship with the disease. ARVD can occur in families; more than 9 different chromosomal defects have been described, most often with autosomal dominant inheritance.
One unique form of ARVD, called Naxos disease (after the Greek island where it was first diagnosed), has an autosomal recessive pattern of inheritance.
Diagnosis ARVC is a difficult diagnosis to make. Therefore, the European Society of Cardiology has created a list of diagnostic criteria for the diagnosis of ARVC[3] (see table).
| Major diagnostic criteria for Arrhythmogenic Right Ventricular Cardiomyopathy[3] |
|---|
|
| Diagnostic criteria that can be diagnosed on the ECG |
|
In 2009 these criteria were updated[4][5], see the table below.
Treatment focuses on avoiding complications.[6]
- Medication:
- Anti-arrhythmics: Sotalol better than Amiodarone.
- ACE-inhibitors to prevent cardiac remodelling
- ICD implantation is recommended for the prevention of sudden cardiac death in patients with ARVC with documented sustained VT or VF who are receiving chronic optimal medical therapy.
- ICD implantation can be considered for the prevention of sudden cardiac death in patients with ARVC with extensive disease, including those with left ventricular involvement, 1 or more affected family member with SCD (Sudden Cardiac Death), or undiagnosed syncope when ventricular tachycardia or ventricular Fibrillation has not been excluded as the cause of syncope, who are receiving chronic optimal medical therapy, and who have reasonable expectation of survival with a good functional status for more than 1 y.
- Radiofrequency ablation can be useful as adjunctive therapy in management of patients with ARVC with recurrent ventricular tachycardia, despite optimal antiarrhythmic drug therapy.
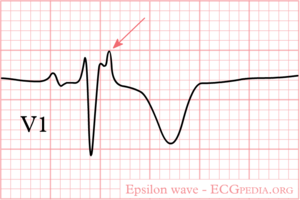
ECG in ARVD
On ARVD.org the latest ECG criteria for ARVD are updated. To enhance detection of ECG abnormalities specific settings to record an ARVD ECG can be used: ECG settings to enhance recording of Epsilon waves.
In patients suspected to have ARVD both a normal 12 lead ECG and a Signal Averaged ECG (SAECG) are useful.
Revised Task Force Criteria ARVD / ARVC
| Original Task Force Criteria | Revised Task Force Criteria |
|---|---|
| I. Global or regional dysfunction and structural alterations∗ | |
| Major | |
|
By 2D echo:
By MRI:
By RV angiography:
|
| Minor | |
|
By 2D echo:
By MRI:
|
| II. Tissue characterization of wall | |
| Major | |
|
|
| Minor | |
| |
| III. Repolarization abnormalities | |
| Major | |
| |
| Minor | |
|
|
| IV. Depolarization/conduction abnormalities | |
| Major | |
|
|
| Minor | |
|
|
| V. Arrhythmias | |
| Major | |
| |
| Minor | |
|
|
| VI. Family history | |
| Major | |
|
|
| Minor | |
|
|
| |
References
- Corrado D, Basso C, and Thiene G. Arrhythmogenic right ventricular cardiomyopathy: diagnosis, prognosis, and treatment. Heart. 2000 May;83(5):588-95. DOI:10.1136/heart.83.5.588 |
- Corrado D, Basso C, and Thiene G. Arrhythmogenic right ventricular cardiomyopathy: an update. Heart. 2009 May;95(9):766-73. DOI:10.1136/hrt.2008.149823 |
- McKenna WJ, Thiene G, Nava A, Fontaliran F, Blomstrom-Lundqvist C, Fontaine G, and Camerini F. Diagnosis of arrhythmogenic right ventricular dysplasia/cardiomyopathy. Task Force of the Working Group Myocardial and Pericardial Disease of the European Society of Cardiology and of the Scientific Council on Cardiomyopathies of the International Society and Federation of Cardiology. Br Heart J. 1994 Mar;71(3):215-8. DOI:10.1136/hrt.71.3.215 |
- Cox MG, van der Smagt JJ, Noorman M, Wiesfeld AC, Volders PG, van Langen IM, Atsma DE, Dooijes D, Houweling AC, Loh P, Jordaens L, Arens Y, Cramer MJ, Doevendans PA, van Tintelen JP, Wilde AA, and Hauer RN. Arrhythmogenic right ventricular dysplasia/cardiomyopathy diagnostic task force criteria: impact of new task force criteria. Circ Arrhythm Electrophysiol. 2010 Apr;3(2):126-33. DOI:10.1161/CIRCEP.109.927202 |
- Marcus FI, McKenna WJ, Sherrill D, Basso C, Bauce B, Bluemke DA, Calkins H, Corrado D, Cox MG, Daubert JP, Fontaine G, Gear K, Hauer R, Nava A, Picard MH, Protonotarios N, Saffitz JE, Sanborn DM, Steinberg JS, Tandri H, Thiene G, Towbin JA, Tsatsopoulou A, Wichter T, and Zareba W. Diagnosis of arrhythmogenic right ventricular cardiomyopathy/dysplasia: proposed modification of the Task Force Criteria. Eur Heart J. 2010 Apr;31(7):806-14. DOI:10.1093/eurheartj/ehq025 |
- European Heart Rhythm Association, Heart Rhythm Society, Zipes DP, Camm AJ, Borggrefe M, Buxton AE, Chaitman B, Fromer M, Gregoratos G, Klein G, Moss AJ, Myerburg RJ, Priori SG, Quinones MA, Roden DM, Silka MJ, Tracy C, Smith SC Jr, Jacobs AK, Adams CD, Antman EM, Anderson JL, Hunt SA, Halperin JL, Nishimura R, Ornato JP, Page RL, Riegel B, Priori SG, Blanc JJ, Budaj A, Camm AJ, Dean V, Deckers JW, Despres C, Dickstein K, Lekakis J, McGregor K, Metra M, Morais J, Osterspey A, Tamargo JL, Zamorano JL, American College of Cardiology, American Heart Association Task Force, and European Society of Cardiology Committee for Practice Guidelines. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology/American Heart Association Task Force and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death). J Am Coll Cardiol. 2006 Sep 5;48(5):e247-346. DOI:10.1016/j.jacc.2006.07.010 |