Puzzle 2006 9 315 Answer
| Author(s) | A.A.M. Wilde, R.H.J. Peters | |
| NHJ edition: | 2006:09,315 | |
| These Rhythm Puzzles have been published in the Netherlands Heart Journal and are reproduced here under the prevailing creative commons license with permission from the publisher, Bohn Stafleu Van Loghum. | ||
| The ECG can be enlarged twice by clicking on the image and it's first enlargement | ||
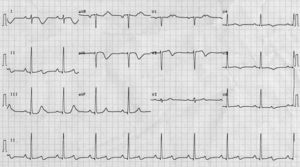
A 63-year-old lady presented with episodic chest pain without specific triggers (in particular no relation with exercise). Physical examination revealed no abnormalities. The ECG is shown in figure 1. An echo was normal and so were the coronary arteries upon coronary angiography. Her family history revealed no coronary artery disease, sudden death, epilepsia or syncope. She herself had never had a syncopal episode either.
A causal reason for the chest pain could not be identified. Coronary artery disease seems unlikely. The abnormalities on the ECG persisted during the admission period which lasted a couple of days.
What to do?
Answer
At first glance the ECG shows a sinus rhythm of 53 beats/min (RR 1140 according to the computer analysis). The electrical axis is vertical (95°). The PQ interval is slightly prolonged (220 msec). The QRS width is within normal limits. Repolarisation is grossly abnormal and significantly prolonged. In the first complex of lead aVL, for example, it measures 600 ms (QTc 567 ms).
A second look at the ECG suggests the presence of a double P-wave frequency, best seen in the usual leads where sinus P waves are most prominent, i.e. lead II (rhythm strip) and lead V1. Hence, the correct diagnosis should be a sinus rhythm of 106 beats/min, 2:1 atrioventricular block and significant QT prolongation. The AV block worsened episodically during telemetry recording.
The question that now should arise is whether the QT prolongation is congenital or acquired. Different factors causally involved in acquired LQTS were not present, except for the female gender and the slight bradycardia. However, the latter is not very pronounced and most likely caused by a functional AV block. The second P wave is not able to conduct through the AV node because the ventricles are still refractory secondary to the prolonged QT interval. This electrocardiographic appearance actually makes a congenital QT prolongation far more likely.
In conclusion, this ECG suggests the presence of an apparent asymptomatic congenital LQTS. Since the bradycardia plays an important role, DDD-PM implantation is warranted as well as DNA diagnostics. The latter should primarily be directed at the SCN5a gene, the gene encoding the cardiac sodium channel and involved in long-QT syndrome, Brugada syndrome and conduction disorders.