Puzzle 2005 5 189 - Answer
| Author(s) | A.A.M. Wilde | |
| NHJ edition: | 2005:5,189 | |
| These Rhythm Puzzles have been published in the Netherlands Heart Journal and are reproduced here under the prevailing creative commons license with permission from the publisher, Bohn Stafleu Van Loghum. | ||
| The ECG can be enlarged twice by clicking on the image and it's first enlargement | ||
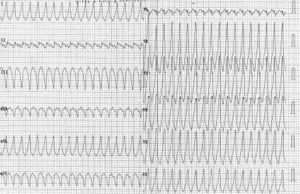
A 65-year-old male presented with palpitations and dizziness of sudden onset, without any associated chest pain or other symptoms. His medical history includes an inferior myocardial infarction three years ago, treated with primary percutaneous transluminal coronary angioplasty (PTCA). No acute complications were reported and he had been without symptoms ever since. With the exception of a low blood pressure (90/60 mmHg), physical examination reveals no abnormalities. His ECG is shown in figure 1 (standard calibrations).
What is your diagnosis?
Answer
The ECG shows a broad QRS complex tachycardia (QRS width 130 ms). The RR intervals are 280 ms (heart rate 214 beats/min). The electrical axis is in the left upper quadrant (leftward shift). There is a left bundle branch block morphology (negative complex in lead V1) with positive complexes in the other precordial leads.
In the differentiation between ventricular tachycardia and supraventricular tachycardia with aberrant conduction, the position of eventual P waves is crucial. The most optimal leads to look at for P waves are leads II and V1. A close look at lead II reveals a negative P wave after every second QRS complex: before the first QRS complex, after the 2nd QRS complex, after the 4th, etcetera (figure 2) which is an enlarged version of lead II. These negatives P waves are most likely retrograde P waves in the presence of 2:1 ventriculoatrial (VA) dissociation. And this is a strong argument for ventricular tachycardia (specificity 98%, sensitivity 66%, Brugada et al. [1]). The origin of the tachycardia is most likely the inferior part of the intraventricular septum, compatible with a history of an inferior wall MI.
Conclusion, the correct diagnosis is ventricular tachycardia with 2:1 VA dissociation.
References
<biblio>
- brugada pmid=2022022
<biblio>