Palpitations after a MAZE Procedure
| Author(s) | A.A.M. Wilde, H.H.D. Idzerda | |
| NHJ edition: | 2005:02,72 | |
| These Rhythm Puzzles have been published in the Netherlands Heart Journal and are reproduced here under the prevailing creative commons license with permission from the publisher, Bohn Stafleu Van Loghum. | ||
| The ECG can be enlarged twice by clicking on the image and it's first enlargement | ||
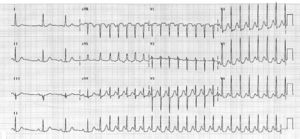
A 75-year-old lady presented with palpitations. Her medical history reveals cardiac surgery with a mitral valve repair combined with a MAZE procedure two years prior to presentation. In the past two years she had been without complaints. The current palpitations are associated with dizziness, and a general uncomfortable feeling. Upon physical examination blood pressure is normal and the pulse is regular at 190 beats/min. Because of the high rate, the heart sounds could not be interpreted. The ECG at presentation is shown in figure 1. Vagal manoeuvres were not effective nor was adenosine up to a dose of 18 mg.
What is your diagnosis?
The initial four beats on the electrocardiogram are compatible with sinus rhythm at a slightly irregular rate. After the 4th beat an extrasystole initiates a narrow QRS complex tachycardia with a cycle length of 340 ms (rate of ±180 beats/min). The initiating P wave has a different morphology than the sinus P wave. Its morphology is (also) positive in the inferior leads and negative in lead aVL, indicating a left atrial superior origin. The same P wave is presumably superimposed on the T wave of the subsequent beats (in lead aVL the negative P wave seems clearly discernable). Based on the morphology of the P wave the most likely diagnosis is a left atrial tachycardia, which is not an uncommon finding after a MAZE procedure. An alternative diagnosis could be AV nodal reentrant tachycardia but this is usually initiated by an atrial extrasystole with a long PR interval (the ‘slow pathway’) followed by a retrograde P wave (conducted through the ‘fast pathway’). The morphology and timing of the P wave are not compatible with common type AV nodal reentrant tachycardia or uncommon type AV nodal reentrant tachycardia (the morphology in particular). An orthodromic AV reentry tachycardia (with a concealed bypass) is not likely either because of the presumable positive P wave in the inferior leads. In summary, the most likely diagnosis is a left atrial tachycardia post MAZE procedure.