Mechanisms of Arrhythmias: Difference between revisions
m (New page: =Principles of Arrhythmias= ==Abnormal impulse formation== Abnormal impulse formation can result in an abnormal frequency, as in symptomatic sinusbradycardia, but oft...) |
mNo edit summary |
||
| (6 intermediate revisions by 2 users not shown) | |||
| Line 1: | Line 1: | ||
[[file:arrhythmia-mechanisms.svg|thumb|Mechanisms of arrhythmias]] | |||
==Abnormal impulse formation== | ==Abnormal impulse formation== | ||
Abnormal impulse formation can result in | Abnormal impulse formation can result in abnormal frequency, as in symptomatic [[#sinus bradycardia|sinus bradycardia]], but often the problem is an abnormal location of impulse formation, as is the cause in an [[#ectopic_pacemaker|ectopic pacemaker]]. | ||
===Abnormal automaticity=== | ===Abnormal automaticity=== | ||
The sinus node contains pacemaker cells that have spontaneous firing capacity | The sinus node contains pacemaker cells that have spontaneous firing capacity. This is called ''normal automaticity''. '''Abnormal automaticity''' occurs when other cells start firing spontaneously, resulting in premature heartbeats. All cardiac cells have spontaneous firing capacity, but at only at a very slow heart rate. Therefore, during a normal heart rate, they will never have the chance to show off their firing capacity. However, in pathologic conditions, such as during extreme bradycardia, other cells can take over and cause for example an [[AV nodal rhythm|AV-nodal heart rate]]. | ||
{{clr}} | {{clr}} | ||
===Triggered activity=== | ===Triggered activity=== | ||
''' | During '''triggered activity''' heart cells contract twice, although they only have been activated once. This is often caused by so called ''afterdepolarizations'' (early or delayed afterdepolarizations EADs / DADs) caused by electrical instability in the myocardial cell membrane. A typical example of this is [[Torsade de Pointes]]. | ||
{{clr}} | {{clr}} | ||
==Abnormal conduction== | ==Abnormal conduction== | ||
===Conduction delay=== | ===Conduction delay=== | ||
| Line 14: | Line 15: | ||
===Re-entry=== | ===Re-entry=== | ||
[[Image: | [[Image:Re-entry.svg|thumb|'''Re-entry'''. A prerequisite for re-entry is the presence of two pathways with differing conduction velocities that connect two points, in this case the atria with the ventricles. The signal splits in two at arrival, but no arrhythmia is initiated as the slow signal becomes extinct when it meets the fast signal. However, after an extrasystole (second image) the fast pathway is still refractory and conduction is by the slow pathway, resulting in a prolongation of the PR interval. The signal that reaches the His by the slow pathway may find the fast pathway conducting and return to the atria (third image), resulting in an '''echo beat'''. This may set in motion a re-entry pathway through the AV node resulting in AV nodal tachycardia (fourth image).]] | ||
[[Image:re-entry2.svg|thumb]] | |||
Re-entry is a common cause of arrhythmias. [[#Ventricular tachycardia|Ventricular tachycardia]] and [[#AVNRT|AV-nodal re-entry]] are typical examples. Re-entry can occur when a conduction path is partly slowed down. As a result of this, the signal is conducted by both a fast and a slow pathway. During normal sinus rhythm this generally does not cause problems, but when an extrasystole follows rapidly upon the previous beat, the fast pathway is sometimes still refractory and cannot conduct the signal. Now the following sequence results in re-entry. | Re-entry is a common cause of arrhythmias. [[#Ventricular tachycardia|Ventricular tachycardia]] and [[#AVNRT|AV-nodal re-entry]] are typical examples. Re-entry can occur when a conduction path is partly slowed down. As a result of this, the signal is conducted by both a fast and a slow pathway. During normal sinus rhythm this generally does not cause problems, but when an extrasystole follows rapidly upon the previous beat, the fast pathway is sometimes still refractory and cannot conduct the signal. Now the following sequence results in re-entry. | ||
# The atrial signal coming from above is conducted by the slow pathway | # The atrial signal coming from above is conducted by the slow pathway. | ||
# As the signal through the slow pathway reaches the end of the fast pathway, it finds this pathway | # As the signal, going through the slow pathway, reaches the end of the fast pathway, it finds this pathway able to conduct. | ||
# The signal is conducted through the fast pathway up to the beginning of the slow pathway, which by that time is | # The signal is conducted through the fast pathway up to the beginning of the slow pathway, which by that time is able to conduct. | ||
# This circle is perpetuated and a signal generator is created. In the case of [[#AVNRT|AV-nodal re-entry]] this will typically generate a signal at a frequency of 180-250 bpm. | # This circle is perpetuated and a signal generator is created. In the case of [[#AVNRT|AV-nodal re-entry]] this will typically generate a signal at a frequency of 180-250 bpm. | ||
{{clr}} | {{clr}} | ||
Latest revision as of 12:04, 22 April 2010
Abnormal impulse formation
Abnormal impulse formation can result in abnormal frequency, as in symptomatic sinus bradycardia, but often the problem is an abnormal location of impulse formation, as is the cause in an ectopic pacemaker.
Abnormal automaticity
The sinus node contains pacemaker cells that have spontaneous firing capacity. This is called normal automaticity. Abnormal automaticity occurs when other cells start firing spontaneously, resulting in premature heartbeats. All cardiac cells have spontaneous firing capacity, but at only at a very slow heart rate. Therefore, during a normal heart rate, they will never have the chance to show off their firing capacity. However, in pathologic conditions, such as during extreme bradycardia, other cells can take over and cause for example an AV-nodal heart rate.
Triggered activity
During triggered activity heart cells contract twice, although they only have been activated once. This is often caused by so called afterdepolarizations (early or delayed afterdepolarizations EADs / DADs) caused by electrical instability in the myocardial cell membrane. A typical example of this is Torsade de Pointes.
Abnormal conduction
Conduction delay
Conduction delay can cause a slow heart rate, as happens during AV conduction blocks. If conduction delay occurs more distally in the heart, i.e. within the ventricles, the QRS complex will widen and a left or right bundle branch block can be seen on the ECG.
Re-entry
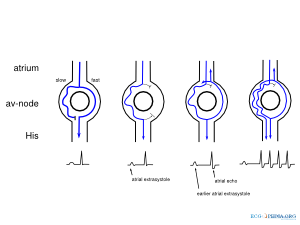
Re-entry is a common cause of arrhythmias. Ventricular tachycardia and AV-nodal re-entry are typical examples. Re-entry can occur when a conduction path is partly slowed down. As a result of this, the signal is conducted by both a fast and a slow pathway. During normal sinus rhythm this generally does not cause problems, but when an extrasystole follows rapidly upon the previous beat, the fast pathway is sometimes still refractory and cannot conduct the signal. Now the following sequence results in re-entry.
- The atrial signal coming from above is conducted by the slow pathway.
- As the signal, going through the slow pathway, reaches the end of the fast pathway, it finds this pathway able to conduct.
- The signal is conducted through the fast pathway up to the beginning of the slow pathway, which by that time is able to conduct.
- This circle is perpetuated and a signal generator is created. In the case of AV-nodal re-entry this will typically generate a signal at a frequency of 180-250 bpm.