LBBB: Difference between revisions
mNo edit summary |
|||
| (7 intermediate revisions by 5 users not shown) | |||
| Line 1: | Line 1: | ||
<onlyinclude>{{Box| | |||
;Criteria for left bundle branch block (LBBB) <cite>Garcia</cite> | ;Criteria for left bundle branch block (LBBB) <cite>Garcia</cite> | ||
:QRS >0,12 sec | :QRS >0,12 sec | ||
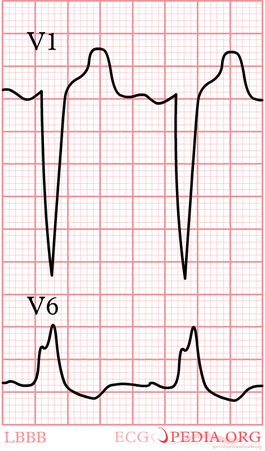
:Broad monomorphic R waves in I and V6 with no Q waves | :Broad monomorphic R waves in I and V6 with no Q waves | ||
:Broad monomorphic S waves in V1, may have a small r wave | :Broad monomorphic S waves in V1, may have a small r wave | ||
}} | |||
{| align="right" | |||
|- | |||
| | |||
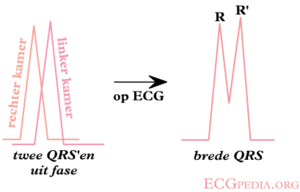
[[Image:Ontstaan_LBTB.png|thumb| In a LBBB, the left ventricle is depolarized later than the right ventricle.]] | [[Image:Ontstaan_LBTB.png|thumb| In a LBBB, the left ventricle is depolarized later than the right ventricle.]] | ||
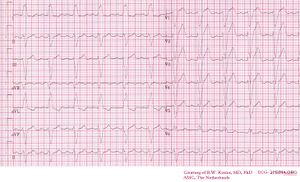
[[Image:12leadLBTB.png|thumb| Left bundle branch Block on a 12 lead ECG.]] | [[Image:12leadLBTB.png|thumb| Left bundle branch Block on a 12 lead ECG.]] | ||
[[Image:12leadLBTB002.jpg|thumb| Another example of Left bundle branch Block on a 12 lead ECG.]] | |||
| | |||
[[Image:LBBB.png|thumb|265px| In a LBBB, the last depolarization wave is in the left ventricle. This wave is directed away from V1. On the ECG, V1 will show a negative complex.]] | |||
|} | |||
In ''left bundle branch block'' (LBBB) the conduction in the left bundle is slow. This results in delayed depolarization of the left ventricle, especially the left lateral wall. The electrical activity in the left lateral wall is unopposed by the usual right ventricular electrical activity. The last activity on the ECG thus goes to the left or away from V1. Once you remember this, LBBB is easy to understand. | |||
[[MI Diagnosis in LBBB|Diagnosis of myocardial infarction in LBBB]] can be difficult. | |||
==Other definitions== | |||
The above definition of left bundle branch block is rather broad. In selecting patients for '''CRT-D therapy''' (cardiac resynchronization therapy) there has been debate whether a more specific definition should be used. In the RAFT trial the following AHA/ESC definition was used<cite>Tang</cite><cite>ESC-ECG</cite>: | |||
{{clr}} | '''Complete LBBB''' | ||
#QRS duration greater than or equal to 120 ms in adults, greater than 100 ms in children 4 to 16 years of age, and greater than 90 ms in children less than 4 years of age. | |||
#Broad notched or slurred R wave in leads I, aVL, V5, and V6 and an occasional RS pattern in V5 and V6 attributed to displaced transition of QRS complex. | |||
#Absent q waves in leads I, V5, and V6, but in the lead aVL, a narrow q wave may be present in the absence of myocardial pathology. | |||
#R peak time greater than 60 ms in leads V5 and V6 but normal in leads V1, V2, and V3, when small initial r waves can be discerned in the above leads. | |||
#ST and T waves usually opposite in direction to QRS. | |||
#Positive T wave in leads with upright QRS may be normal (positive concordance). | |||
#Depressed ST segment and/or negative T wave in leads with negative QRS (negative concordance) are abnormal. | |||
#The appearance of LBBB may change the mean QRS axis in the frontal plane to the right, to the left, or to a superior, in some cases in a rate-dependent manner. | |||
'''Incomplete LBBB''' | |||
#QRS duration between 110 and 119 ms in adults, between 90 and 100 ms in children 8 to 16 years of age, and between 80 and 90 ms in children less than 8 years of age. | |||
#Presence of left ventricular hypertrophy pattern. | |||
#R peak time greater than 60 ms in leads V4, V5, and V6. | |||
#Absence of q wave in leads I, V5, and V6. | |||
Also a narrow initial R wave in V1 has been linked with a reduced response to CRT.<cite>Mascioli</cite> | |||
In general when the QRS is wide and the definitions of LBBB and RBBB are not met, the term NIVCD (non-specific intraventricular conduction delay) is used. | |||
Also read [[RBBB|right bundle branch block]]. | |||
{{clr}}</onlyinclude> | |||
{{Box| | |||
==References== | ==References== | ||
<biblio> | <biblio> | ||
#Garcia isbn=0763722464 | #Garcia isbn=0763722464 | ||
#wellens isbn=9781416002598 | #wellens isbn=9781416002598 | ||
#Mascioli pmid=22651702 | |||
#Tang pmid=21073365 | |||
#ESC-ECG pmid=19281930 | |||
</biblio> | </biblio> | ||
}} | |||
Latest revision as of 09:17, 25 August 2012
- Criteria for left bundle branch block (LBBB) [1]
- QRS >0,12 sec
- Broad monomorphic R waves in I and V6 with no Q waves
- Broad monomorphic S waves in V1, may have a small r wave
In left bundle branch block (LBBB) the conduction in the left bundle is slow. This results in delayed depolarization of the left ventricle, especially the left lateral wall. The electrical activity in the left lateral wall is unopposed by the usual right ventricular electrical activity. The last activity on the ECG thus goes to the left or away from V1. Once you remember this, LBBB is easy to understand.
Diagnosis of myocardial infarction in LBBB can be difficult.
Other definitions
The above definition of left bundle branch block is rather broad. In selecting patients for CRT-D therapy (cardiac resynchronization therapy) there has been debate whether a more specific definition should be used. In the RAFT trial the following AHA/ESC definition was used[2][3]:
Complete LBBB
- QRS duration greater than or equal to 120 ms in adults, greater than 100 ms in children 4 to 16 years of age, and greater than 90 ms in children less than 4 years of age.
- Broad notched or slurred R wave in leads I, aVL, V5, and V6 and an occasional RS pattern in V5 and V6 attributed to displaced transition of QRS complex.
- Absent q waves in leads I, V5, and V6, but in the lead aVL, a narrow q wave may be present in the absence of myocardial pathology.
- R peak time greater than 60 ms in leads V5 and V6 but normal in leads V1, V2, and V3, when small initial r waves can be discerned in the above leads.
- ST and T waves usually opposite in direction to QRS.
- Positive T wave in leads with upright QRS may be normal (positive concordance).
- Depressed ST segment and/or negative T wave in leads with negative QRS (negative concordance) are abnormal.
- The appearance of LBBB may change the mean QRS axis in the frontal plane to the right, to the left, or to a superior, in some cases in a rate-dependent manner.
Incomplete LBBB
- QRS duration between 110 and 119 ms in adults, between 90 and 100 ms in children 8 to 16 years of age, and between 80 and 90 ms in children less than 8 years of age.
- Presence of left ventricular hypertrophy pattern.
- R peak time greater than 60 ms in leads V4, V5, and V6.
- Absence of q wave in leads I, V5, and V6.
Also a narrow initial R wave in V1 has been linked with a reduced response to CRT.[4]
In general when the QRS is wide and the definitions of LBBB and RBBB are not met, the term NIVCD (non-specific intraventricular conduction delay) is used.
Also read right bundle branch block.
References
- ISBN:0763722464
- Tang AS, Wells GA, Talajic M, Arnold MO, Sheldon R, Connolly S, Hohnloser SH, Nichol G, Birnie DH, Sapp JL, Yee R, Healey JS, Rouleau JL, and Resynchronization-Defibrillation for Ambulatory Heart Failure Trial Investigators. Cardiac-resynchronization therapy for mild-to-moderate heart failure. N Engl J Med. 2010 Dec 16;363(25):2385-95. DOI:10.1056/NEJMoa1009540 |
- Surawicz B, Childers R, Deal BJ, Gettes LS, Bailey JJ, Gorgels A, Hancock EW, Josephson M, Kligfield P, Kors JA, Macfarlane P, Mason JW, Mirvis DM, Okin P, Pahlm O, Rautaharju PM, van Herpen G, Wagner GS, Wellens H, American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology, American College of Cardiology Foundation, and Heart Rhythm Society. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part III: intraventricular conduction disturbances: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. Endorsed by the International Society for Computerized Electrocardiology. J Am Coll Cardiol. 2009 Mar 17;53(11):976-81. DOI:10.1016/j.jacc.2008.12.013 |
- Mascioli G, Padeletti L, Sassone B, Zecchin M, Lucca E, Sacchi S, Boggian G, Tondo AL, Belvito C, Bakhtadze N, Borrelli A, and Sinagra G. Electrocardiographic criteria of true left bundle branch block: a simple sign to predict a better clinical and instrumental response to CRT. Pacing Clin Electrophysiol. 2012 Aug;35(8):927-34. DOI:10.1111/j.1540-8159.2012.03427.x |
- ISBN:9781416002598