File:E0007082.jpg
Original file (2,644 × 1,599 pixels, file size: 3.41 MB, MIME type: image/jpeg)
Summary
| Description |
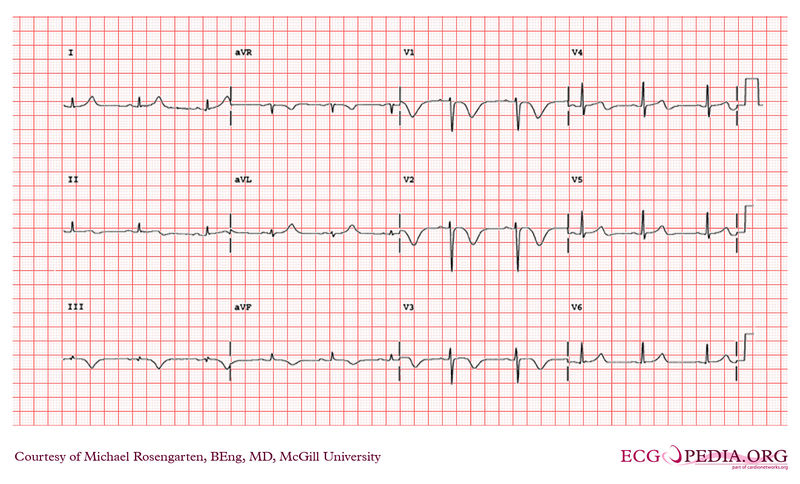
A 47 year old male smoker was brought to the emergency room after having experienced chest discomfort and shortness of breath, followed by a syncopal episode. He had been investigated two weeks earlier for chest pain on exertion (this included a negative exercise stress test which reached 11 mets). In the emergency room, he was short of breath (breathing at 40/min. and requiring 100% oxygen to maintain an adequate saturation) and had a depressed level of consciousness. He was pale and diaphoretic, with a pulse of 120 bpm and a blood pressure of 70 mmHg systolic. His respiratory, cardiac, and abdominal exam were all within normal limits with the exception of the increased heart and respiratory rates. There was no obvious swelling of his lower extremities. An ECG revealed a RBBB not present on previous ECGs. A CXR revealed no failure or other pathology. With resuscitative measures underway, the patient was immediately brought to the cardiac catheterization suite with a working diagnosis of cardiogenic shock secondary to an acute myocardial infarction or acute pulmonary embolism. In the cath lab, the patient became asystolic and ACLS protocol was begun. The patient was intubated and a transvenous pacemaker was inserted. The patient's blood pressure remained low despite maximum infusion of pressors, and thus an intra-aortic balloon pump was inserted. A coronary angiogram was then performed, which revealed completely normal coronary arteries. It was decided at this point to immediately perform a pulmonary angiogram. This revealed massive bilateral pulmonary emboli. One hundred milligrams of rTPA and heparin were given intravenously, with minimal resolution of the emboli. After attempts to mechanicaly break up the emboli were unsuccessful, it was decided to bring the patient to the OR. On the way to the OR, the patient again became asystolic. A median sternotomy was performed, open cardiac massage was begun, and the patient was placed on cardiopulmonary bypass, using right atrial dual caval and ascending aortic cannulation. The heart subsequently began to contract, but the right ventricle was severely hypokinetic. The SVC and IVC were snared, and a longitudinal incision was made in the pulmonary artery (PA). Large amounts of fresh clots were removed from the right PA and multiple small clots were removed from the left PA. Embolectomy catheters were placed down each main PA, but no further clot was obtained. The arteriotomy was closed and attempts at weaning from cadiopulmonary bypass where made. At this point, the RV was massively dilated and severely hypokinetic. Despite maximum inotropes and the intra-aortic balloon pump, the patient was unable to be weaned from bypass. The patient expired due to right ventricular failure, 4 hours after presentation. An autopsy done revealed four chamber cardiac failure, massive pulmonary edema, and endocardial hemorrhages in the RA, RV, and LV, as well as residual organizing thrombus in the left and right PA. |
|---|---|
| Category | |
| Source |
EKG World Encyclopedia http://cme.med.mcgill.ca/php/index.php , courtesy of Michael Rosengarten BEng, MD.McGill |
| Date |
2012 |
| Author |
Michael Rosengarten BEng, MD.McGill |
| Permission |
Creative Commons Attribution Noncommercial Share-Alike License |
File history
Click on a date/time to view the file as it appeared at that time.
| Date/Time | Thumbnail | Dimensions | User | Comment | |
|---|---|---|---|---|---|
| current | 07:19, 10 February 2012 |  | 2,644 × 1,599 (3.41 MB) | DarrelC (talk | contribs) |
You cannot overwrite this file.
File usage
The following page uses this file: