Basics: Difference between revisions
m (→Leadreversals) |
No edit summary |
||
| Line 131: | Line 131: | ||
*'''III''' from the left arm to the left leg | *'''III''' from the left arm to the left leg | ||
An easy rule to remember: lead '''I''' + lead '''III''' = lead '''II''' | An easy rule to remember: lead '''I''' + lead '''III''' = lead '''II''' | ||
This is doen with the use of the height or depth, independent of the wave (QRS, P of T). | |||
Example: if in lead I, the QrS complex is 3 mm in height and in lead III 9mm, the height of the QRS-complex in lead II is 12mm. | |||
Other exttremity leads are: | |||
*'''AVL''' | *'''AVL''' points to the left arm | ||
*'''AVR''' | *'''AVR''' points to the right arm | ||
*'''AVF''' | *'''AVF''' points to the feet | ||
The capital A stands for "augmented" and V for "voltage". | |||
(aVR + aVL + aVF = 0) | (aVR + aVL + aVF = 0) | ||
| Line 173: | Line 173: | ||
**omkering van afleidingen aVR en aVF | **omkering van afleidingen aVR en aVF | ||
Men kan draadverwisseling en [[wikipedia:Dextrocardia| | Men kan draadverwisseling en [[wikipedia:Dextrocardia|dextrocardia]] van elkaar onderscheiden door eveneens naar de precordiale afleidingen te kijken. Dextrocardia toont R-golf inversie i.t.t. omkering van de electroden. | ||
==Disturbances== | ==Disturbances== | ||
Revision as of 11:45, 12 May 2007
Some statements may be disputed, incorrect or biased. |
Introduction
The aim of this course is to understand and recognize the normal ECG and to be able to interprete abnormalities. The course is divided in different sections. First the basics will be presented. This is followed by the interpretation of the normal ECG. Then abnormalities are discussed: (ischemia, arrhythmias and Miscellaneous). Finally the real world is presented in practice ECGs.
The American College of Cardiology has published a list of abnormalities a professional should be able to recognise. It is advisable to go through this list at the end of this course in order to recognise areas that need your attention.
How do I begin reading an ECG?
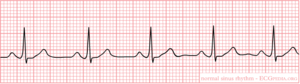
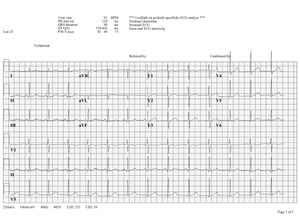
Click on the ECG to see an enlargement. Where do we look when watching an ECG?
- top left are the patient's information, name, sex and date of birth
- at the right of that are below each other the heart frequency, the conduction time intervals (PQ,QRS,QT/QTc), and the cardiac axis (P-top axis, QRS axis and T-top axis)
- further to the right is the interpretation of the ECG written (this often misses in a 'fresh' ECG, but later the interpretation of the cardiologist or computer will be added)
- down left is the 'paper speed' (25mm/s on the horizontal ax), the sensitivity (10mm/mV) and the filter's frequency (40Hz, filters noise from eg. lights)
- finally there is a calibration on the ECG, on the beginning of every lead is a vertical block that shows how high 1mV is. So the height and depth of these signals are a measurement for the voltage. If this is not the set 10mm, there is something wrong with the machine.
- further we have the ECG leads themselves of course, these will be discussed below.
Note that the lay-out is different for every machine, but all of the information above can be found.
What does the ECG register?
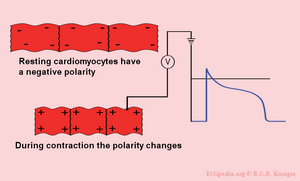
An ECG is a registration of the heart's electric activity.
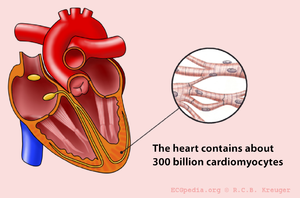
Just like skeletal muscles, the heart is electrically stimulated to contract. This stimulation is also called activation or excitation. Cardiac muscles are electrically charged in rest. The surface of the cell is positively charged relative to the inside (resting potential). If the cardiac muscle cells are electrically stimulated (depolarisation: the outside of the depolarized region is positively charged relative to the inside) and there comes an action potential, the cells contract. Because of the spreading of the impulse through the heart, the electric field changes continually in size and direction. The ECG is a graphical visualisation of the electric signals in the heart.
The ECG is a sum of the action potentials from millions of cardiomyocytes
| width=382|height=315|quality=best|align=right | </flash> |
|---|---|
| This movie shows the contraction of a single (rabbit)heartcell. The glass electrode measures the electrical current in the heartcell(according to thepatch-clamp method). The electrical signal is written in blue and shows the actionpotential. Courtesy of Arie Verkerk and Antoni van Ginneken. |
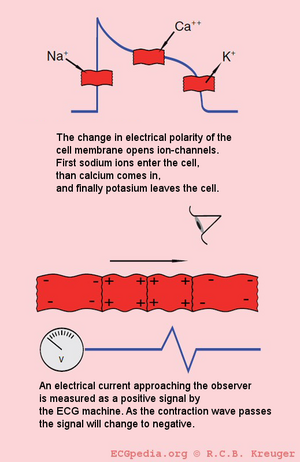
The individual action potentials of the individual cardiomyocytes are averaged. The final result which is shown on the ECG is actually the average of trillions of microscopic electronical signals.
The electric discharge of the heart
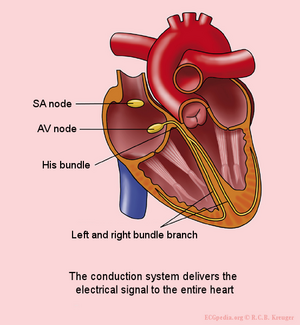
In the sinal node (SA node) are pacemakercells which determine the heart frequency.
First the atria depolarise and contract, after that the ventricles
The electrical signal between the atria and the ventricles goes from the sinus node, via the atria to the AV-node (atrioventricular transition) to the His bundle and subsequently to the right and left bundle branch, which end in a dense network of Purkinje fibers.
The different ECG waves
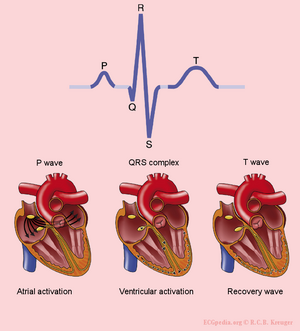
The P wave is the result of the atrial depolarization. This depolarization starts in the SA (sino-atrial) node. The signal produces by pacemakercells in the SA node is conducted by the conduction system to the right and left atria. Normal atrial repolarisation is not visible on the ECG (but can be visible during atrial infarction and pericarditis).
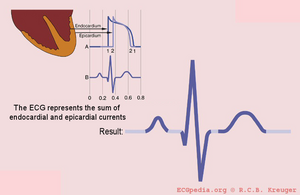
The QRS complex is the average of the depolarization waves of the inned (endocardioal) and outer (epicardial) cardiomyocytes. As the endocardial cardiomyocytes depolarize slightly earlier than the outer layers, a typical QRS pattern occurs (figure).
The T wave represents the repolarisation of the ventricles. There is no cardiac muscle activity during the T wave.
One heart beat consists of a atrial depolarization --> atrial contraction --> p-wave, ventricular depolarization --> ventricular contraction --> ORS-complex and the resting phase (including the repolarization during the T-wave) between two heart beats.
Have a look at this excellent [animation of the heart cycle]
The origin of the U wave is unknown. This wave possibly results from "afterdepolarizations" of the ventricles.
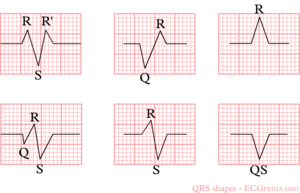
The letters "Q", "R" and "S" are used to describe the QRS complex:
- Q: the first negative deflection after the p-wave. If the first deflection is not negative, the Q is absent.
- R: the positive deflection
- S: the negative deflection after the R-wave
- small print letters (q, r, s) are used to describe deflections of small amplitude. For example: qRS = small q, high R, deep S.
- R`: i used to describe a second R-wave (as in a [[right bundlebranch block])
See figure for some examples of this.
The history of the ECG


The history of the ECG goes back more than one and a half century
In 1843 Emil Du Bois-Reymond, a german physiologist, was the to describe "action potentials" of muscular contraction. He used a highly sensitive galvanometer, which contained more than 5 km of wire. Du Bios Reymond named the different waves: "o" was the stable equilibrium and he was the first to use the p, q, r and s to describe the different waves. Du Bois-Reymond, E. Untersuchungen uber thierische Elektricitat. Reimer, Berlin: 1848.
In 1850 M. Hoffa described how he could induce irregular contractions of the ventricles of doghearts by administering electrical shock. Hoffa M, Ludwig C. 1850. Einige neue versuche uber herzbewegung. Zeitschrift Rationelle Medizin, 9: 107-144
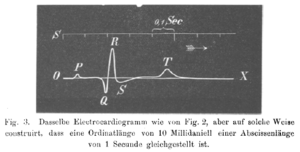
In 1887 the English physiologist Augustus D. Waller from Londen published the first human electrocardiogram. He used a capillar-electrometer. Waller AD. A demonstration on man of electromotive changes accompanying the heart's beat. J Physiol (London) 1887;8:229-234
The dutchman Willem Einthoven (1860-1927) introduced in 1893 the term 'electrocardiogram'. He described in 1895 how he used a galvanometer to visualize the electrical activity of the heart. In 1924 he received the Nobelprize for his work on the ECG. He connected electrodes to a patienta showed the electrical difference between two electrodes on the galvanometer. We still now use the term: Einthovens'leads. The string galvanometer (see Image) was the first clinical instrument on the recording of an ECG.
In 1905 Einthoven recorded the first 'telecardiogram' from the hospital to his laboratoy 1.5 km away.
In 1906 Einthoven published the first article in which he described a series of abnormal ECGs: left- and right bundlebranchblock, left- and right atrialdilatation, the U wave, notching of the QRS complex, ventricular extrasystoles, bigemini, atrialflutter and total AV block. Einthoven W. Le telecardiogramme. Arch Int de Physiol 1906;4:132-164
The ECG electrodes
Electric activity going through the heart, can be measured by external (skin)electrodes. The electrocardiogram (ECG) registers these activities from these electrodes which have been attached on diffrent places on the body. In total, twelve leads are calculated using ten electrodes.
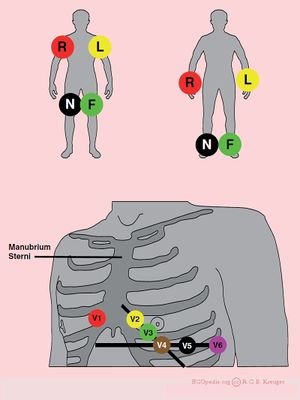
The ten electrodes are:
- the extremity leads:
- LA - left arm
- RA - right arm
- N - neutral, on the right leg (= electrisch aarde of nulpunt ten opzichte waarvan de electrische spanning wordt gemeten)
- F - foot, on the left leg
It makes no difference whether the electrodes are attached proximal or distal on the extremities. However, it is best to be uniform in this. (eg. do not attach an electrode on the left shoulder and one on the right wrist).
- the chest leads:
- V1 - placed in the 4th intercostal space, right of the sternum
- V2 - placed in the 4th intercostal space, left of the sternum
- V3 - placed between V2 and V4
- V4 - placed 5th intercostal space in the nippleline
- V5 - placed between V4 ann V6
- V6 - placed in the axillar line on the same height as V4
Using these 10 electrodes, 12 leads can be derived. There are 6 extremity leads and 6 precordial leads.
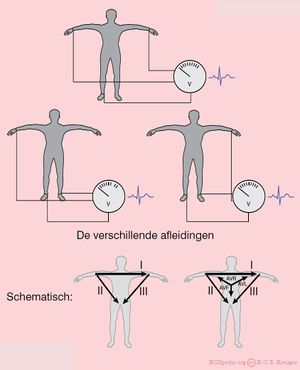
The extremity leads
The extremity leads are:
- I from the right ot the left arm
- II from the right arm to the left leg
- III from the left arm to the left leg
An easy rule to remember: lead I + lead III = lead II This is doen with the use of the height or depth, independent of the wave (QRS, P of T). Example: if in lead I, the QrS complex is 3 mm in height and in lead III 9mm, the height of the QRS-complex in lead II is 12mm.
Other exttremity leads are:
- AVL points to the left arm
- AVR points to the right arm
- AVF points to the feet
The capital A stands for "augmented" and V for "voltage".
(aVR + aVL + aVF = 0)
The chest leads
De voorwandsafleidingen (V1,V2,V3,V4,V5 en V6) 'kijken' vanuit hun borstelectrodes naar het electrisch gemiddelde. Dus in feite naar het centrum van het hart.
Voorbeeld: V1 zit vlakbij de rechter kamer en het rechter atrium en signalen vanuit die gebieden geven in deze afleiding de grootste uitslag. V6 zit vlakbij de laterale (=zijkant) van de linker hartkamer, hier worden signalen vanuit de linker hartkamer het best geregistreerd.
Special leads
Bij een onderwandinfarct worden soms extra afleidingen gebruikt:
- Bij een zogenaamd rechts uitgepoold ECG behouden V1 en V2 hun plaats. V3 tm V6 worden op dezelfde plaats gezet, maar dan langs de rechterkant van het borstbeen. Op het ECG moet aangegeven worden dat het om een Rechts-ECG gaat. V4R (V4 maar dan rechts uitgepoold) is een gevoelige afleiding om een rechterkamerinfarct te diagnostiseren.
- Afleidingen V7-V8-V9 worden gebruikt om een posteriorinfarct aan te tonen. Hierbij wordt doorgepoold ter hoogte van V6 naar de rug. Een posteriorinfarct is meestal ook goed te zien in V2 (maar dan 'op de kop', zie ook het hoofdstuk ischemie, dus deze afleidingen worden zelden gebruikt.
Technical problems with the ECG
Lead reversals
Het komt nogal eens voor dat één van de afleidingsdraden niet goed aangesloten wordt. Het is handig om dit te kunnen herkennen, want anders kan je verkeerde conclusies trekken.
Denk bij een 'vreemd' ECG daarom aan een dradenverwisseling. Een van de meest voorkomende fouten is het verwisselen van de linker en rechter arm. Dit uit zich in een negatieve afleiding in I. Dit zou ook door een rechter asdraai kunnen komen, maar dat is heel zeldzaam.
Veel voorkomende verwisselingen zijn, omkering van:
- rechter en linker arm electroden;
- omkering van afleiding II en III
- omkering van de afleingen aVR en aVL
- linker arm en linker been:
- omkering van afleiding I en II
- omkering van afleiding aVF en aVF
- inversie van sfleiding III
- rechter arm en linker been:
- inversie va afleiding I, II en III
- omkering van afleidingen aVR en aVF
Men kan draadverwisseling en dextrocardia van elkaar onderscheiden door eveneens naar de precordiale afleidingen te kijken. Dextrocardia toont R-golf inversie i.t.t. omkering van de electroden.
Disturbances
- Bewegingsartefacten
- Tremor
- Electrische storing
- Verkeerde filter-instelling