AVNRT: Difference between revisions
mNo edit summary |
mNo edit summary |
||
| (14 intermediate revisions by 4 users not shown) | |||
| Line 2: | Line 2: | ||
{{Arrhythmias| | {{Arrhythmias| | ||
| name = AV Nodal Re-entry Tachycardia (AVNRT) | | name = AV Nodal Re-entry Tachycardia (AVNRT) | ||
| | | locatieafbeelding = | ||
| atrial_frequency = 180-250 bpm | | atrial_frequency = 180-250 bpm | ||
| ventricular_frequency = 180-250 bpm | | ventricular_frequency = 180-250 bpm | ||
| Line 9: | Line 9: | ||
| p_wave = inside or right after the QRS complex | | p_wave = inside or right after the QRS complex | ||
| adenosine = terminates the arrhythmia(!) | | adenosine = terminates the arrhythmia(!) | ||
}} | }} | ||
'''AV Nodal Re-entry Tachycardia (AVNRT)''' or Atrial-Ventricular Nodal Re-entry Tachycardia is a [[SVT|supra-ventricular arrhythmia]] | [[File:Re_entry.svg|thumb|left|[[Re-entry]] as seen in AVNRT]] | ||
'''AV Nodal Re-entry Tachycardia (AVNRT)''' or Atrial-Ventricular Nodal Re-entry Tachycardia is a [[SVT|supra-ventricular arrhythmia]], and more precisely, a nodal arrhythmia. AVNRT is the most frequently occurring form of regular tachycardia. More females than males have signs of AVNRT. The ratio is approximately 3:1. Symptoms are bouts of fast heart rates with sudden onset. Neck vein palpitations can be prominent (the 'Frog Sign'). Termination is often possible with valsalva manouevres (blowing on wrist, squatting, carotid sinus massage) or medication (adenosine, verapamil, diltiazem), or electrocardioversion. An AVNRT is a regular rhythm with a rate of 180-250 /min. A condition for AVNRT to occur is that 2 electric pathways occur in and around the AV node (a slow paced and a fast paced pathway). That gives way to the occurrence of re-entry. | |||
Two forms of | Two forms of AVNRT occur: typical and atypical AVNRT | ||
*'''Typical | *'''Typical AVNRT''' (also described as common AVNRT or slow-fast AVNRT): The impulse travels over the slow pathway towards the ventricles and returns via the fast pathway to the atria. The retrograde P wave (or Atrial echo) shows up at the end of the QRS. 90 % of all patients with AVNRT are diagnosed with typical AVNRT. Spontaneous termination of typical AVNRT often occurs in the fast pathway (terminates with a QRS on the ECG), induced termination with carotid sinus massage or adenosine results in termination in the slow pathway (terminates with retrograde P on ECG). | ||
*'''Atypical ANVRT''' (also described as uncommon AVNRT or fast-slow AVNRT): The impulse travels via the fast pathway towards the ventricles and returns via the slow pathway to the atria. The retrograde P wave appears far behind the QRS. Only about 6% of all ANVRT patients are diagnosed with atypical AVNRT. | |||
*'''Atypical ANVRT''' (also described as uncommon | The remaining cases of AVNRT patients are diagnosed with a form of AVNRT that is even more rare. This form of AVNRT is '''slow/slow AVNRT''' (The impulse follows a complex route through the AV node and the surrounding area). Only 4 % of all patients diagnosed with AVNRT have slow/slow AVNRT. | ||
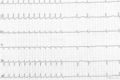
==How does an AVNRT show up on an ECG?== | |||
Two sensitive characteristics to identify AVNRT on the ECG are: | Two sensitive characteristics to identify AVNRT on the ECG are: | ||
* R'. This is a small secondary R wave. It resembles a [[RBBB|right bundle branch block]], but the QRS width stays < 120ms. | * R'. This is a small secondary R wave. It resembles a [[RBBB|right bundle branch block]], but the QRS width stays < 120ms. | ||
* RP << 100ms. The distance between the R and P waves is less than 100ms. | * RP << 100ms. The distance between the R and P waves is less than 100ms. | ||
* Onset after a premature atrial beat with delayed conduction to the ventricles. | |||
{{clr}} | {{clr}} | ||
==Examples== | |||
<gallery> | |||
File:ECG000012.jpg|Another example of AV nodal re-entry tachycardia | |||
Image:avnrt_ecg.jpg|AV Nodal Re-entry Tachycardia (AVNRT) terminated by adenosine injection. Note that the last complex of the tachycardia has a retrograde P wave. Termination by block in the slow pathway is typical for common type AVNRT | |||
Image:avnrt_ecg2.jpg|AV Nodal Re-entry Tachycardia (AVNRT) | |||
</gallery> | |||
Latest revision as of 06:23, 11 December 2012
| This is part of: Supraventricular Rhythms |
| Atrial rate | 180-250 bpm |
| Ventricular rate | 180-250 bpm |
| Regularity | regular |
| Origin | AV node |
| P-wave | inside or right after the QRS complex |
| Effect of adenosine | terminates the arrhythmia(!) |
| Example ECG: {{{example}}} | |
| Example ECG2: {{{example2}}} | |
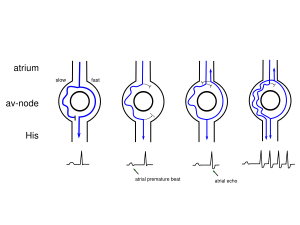
AV Nodal Re-entry Tachycardia (AVNRT) or Atrial-Ventricular Nodal Re-entry Tachycardia is a supra-ventricular arrhythmia, and more precisely, a nodal arrhythmia. AVNRT is the most frequently occurring form of regular tachycardia. More females than males have signs of AVNRT. The ratio is approximately 3:1. Symptoms are bouts of fast heart rates with sudden onset. Neck vein palpitations can be prominent (the 'Frog Sign'). Termination is often possible with valsalva manouevres (blowing on wrist, squatting, carotid sinus massage) or medication (adenosine, verapamil, diltiazem), or electrocardioversion. An AVNRT is a regular rhythm with a rate of 180-250 /min. A condition for AVNRT to occur is that 2 electric pathways occur in and around the AV node (a slow paced and a fast paced pathway). That gives way to the occurrence of re-entry.
Two forms of AVNRT occur: typical and atypical AVNRT
- Typical AVNRT (also described as common AVNRT or slow-fast AVNRT): The impulse travels over the slow pathway towards the ventricles and returns via the fast pathway to the atria. The retrograde P wave (or Atrial echo) shows up at the end of the QRS. 90 % of all patients with AVNRT are diagnosed with typical AVNRT. Spontaneous termination of typical AVNRT often occurs in the fast pathway (terminates with a QRS on the ECG), induced termination with carotid sinus massage or adenosine results in termination in the slow pathway (terminates with retrograde P on ECG).
- Atypical ANVRT (also described as uncommon AVNRT or fast-slow AVNRT): The impulse travels via the fast pathway towards the ventricles and returns via the slow pathway to the atria. The retrograde P wave appears far behind the QRS. Only about 6% of all ANVRT patients are diagnosed with atypical AVNRT.
The remaining cases of AVNRT patients are diagnosed with a form of AVNRT that is even more rare. This form of AVNRT is slow/slow AVNRT (The impulse follows a complex route through the AV node and the surrounding area). Only 4 % of all patients diagnosed with AVNRT have slow/slow AVNRT.
How does an AVNRT show up on an ECG?
Two sensitive characteristics to identify AVNRT on the ECG are:
- R'. This is a small secondary R wave. It resembles a right bundle branch block, but the QRS width stays < 120ms.
- RP << 100ms. The distance between the R and P waves is less than 100ms.
- Onset after a premature atrial beat with delayed conduction to the ventricles.