Puzzle 2006 11 393 Answer
| Author(s) | A.A.M. Wilde, L.R.C. Dekker | |
| NHJ edition: | 2006:11,393 | |
| These Rhythm Puzzles have been published in the Netherlands Heart Journal and are reproduced here under the prevailing creative commons license with permission from the publisher, Bohn Stafleu Van Loghum. | ||
| The ECG can be enlarged twice by clicking on the image and it's first enlargement | ||
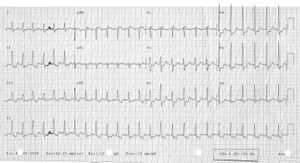
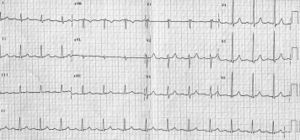
An otherwise healthy 57-year-old lady presented with palpitations without dizziness. The symptoms had been present for a couple of years but the number of episodes had increased recently. Onset and termination were always sudden without specific triggers. Physical examination on admission revealed no specific abnormalities except for a rapid pulse (150 beats/min). Blood pressure was normal. The ECG is shown in figure 1 and a few minutes later figure 2 was recorded without any specific intervention.
What is your diagnosis?
Answer
Figure 1 shows a narrow-complex tachycardia with an RR interval of 390 msec (rate 155 beats/min). In the latter part the arrhythmia is slightly slower (RR interval 410). In the differential diagnosis of any narrowcomplex tachycardia, the position of the P wave (and its number) is critical for the correct diagnosis.
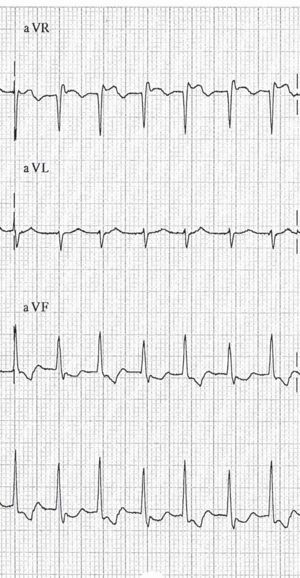
A close look for the P waves reveals a P wave in every other T wave in the left part of the ECG. After the 15th QRS complex, the P wave is present in every T wave (see rhythm strip lead II at the bottom of the ECG and figure 3, arrows). Comparison of the T waves with and without superimposed P waves reveals a negative morphology of the P wave in lead II. In lead aVR the morphology is clearly positive. The timing of the P wave is between 40 and 80 ms after the QRS complex.
The number of P waves indicates a dissociation between the atrial and ventricular rate and the morphology indicates retrograde (VA) conduction. The presence of VA dissociation is only compatible with AV-nodal reentrant tachycardia and it excludes AVreentry tachycardia (orthodromic circus movement tachycardia), atrial tachycardia and atrial flutter, the most important differential diagnostic entities for a narrow-complex tachycardia with the present rate. A rare alternative diagnosis would be a His-bundle tachycardia with 2:1 VA conduction. Actually the position of the P wave would be in favour of this diagnosis.
An invasive electrophysiological study revealed the presence of dual nodal characteristics and, under isoprenaline, the induction of an AV-nodal reentrant tachycardia. Slow pathway ablation successfully modified the arrhythmogenic substrate.