Puzzle 2005 6 244 - Answer
| Author(s) | A.A.M. Wilde, R.B.A. van den Brink | |
| NHJ edition: | 2005:6,244 | |
| These Rhythm Puzzles have been published in the Netherlands Heart Journal and are reproduced here under the prevailing creative commons license with permission from the publisher, Bohn Stafleu Van Loghum. | ||
| The ECG can be enlarged twice by clicking on the image and it's first enlargement | ||
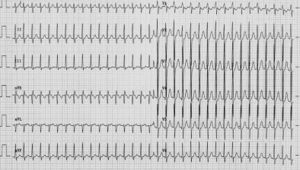
A20-year-old male is having palpitations. They occur without a specific trigger, although episodes are sometimes related to emotion or exercise. Duration is between two minutes and one hour. He does not feel well during an attack, but has never fainted. Physical examination reveals no abnormalities nor does laboratory investigation or echocardiography. His baseline ECG is normal (not shown). He was asked to come to the emergency room if an episode lasted long enough, which he did (figure 1).
Upon presentation during an attack the ECG recorded a narrow-complex tachycardia with an RR interval of 280 msec (214 beats/min). There is a slight rightward deviation of the electrical axis. ST morphology is normal and no P wave can be identified. The differential diagnosis is:
- atrioventricular nodal reentry tachycardia (AVNRT),
- orthodromic tachycardia with a concealed bypass (AVRT) and
- atrial tachy-cardia. Adenosine was administered and the ECG presented in figure 2 was recorded.
What is your diagnosis and what would your further treatment be?
Answer
Figure 2 shows a narrow complex rhythm, with an RR interval of 560 msec, i.e. a rate exactly half of that before adenosine. P waves are now clearly discernable with an axis compatible with sinus rhythm. This suggests either sinus rhythm, or a supraventricular tachycardia with 2:1 block in the AV node caused by adenosine and comparable P wave morphology. AVRT can be excluded as a 1:1 relation between atrium and ventricle is required. AVNRT with 2:1 block to the ventricle is also highly unlikely because of the morphology of the P waves, which in that case would be negative in the inferior leads due to retrograde activation of the atrium. The only remaining alternative is atrial tachycardia from an area in the vicinity of the sinus node. Indeed, on closer examination there is evidence of a second P wave partly hidden in the terminal part of the T wave in lead V1. Shortly after this ECG was obtained the tachycardia (figure 1) resumed. A higher dose of adenosine terminated the tachycardia and sinus rhythm (60 beats/min) appeared. Atrial tachycardias occasionally respond to adenosine. In those cases the underlying electrophysiological mechanism is triggered activity based on delayed afterdepolarisations.[1][2] These tachycardias usually respond well to β-blockade or verapamil, and are generally amenable to catheter ablation.
References
- Markowitz SM, Stein KM, Mittal S, Slotwiner DJ, and Lerman BB. Differential effects of adenosine on focal and macroreentrant atrial tachycardia. J Cardiovasc Electrophysiol. 1999 Apr;10(4):489-502. DOI:10.1111/j.1540-8167.1999.tb00705.x |
- Lerman BB, Stein KM, and Markowitz SM. Adenosine-sensitive ventricular tachycardia: a conceptual approach. J Cardiovasc Electrophysiol. 1996 Jun;7(6):559-69. DOI:10.1111/j.1540-8167.1996.tb00563.x |