Atrial Premature Complexes
| This is part of: Supraventricular Rhythms |
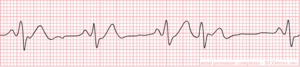
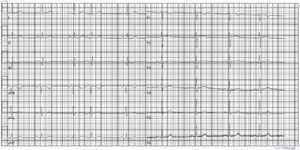
Premature atrial complexes origin from an ectopic pacing region in the atria. They are an example of ectopic beats. The result is a p-wave with often a different morphology from the preceding ones.
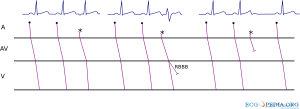
If a premature atrial complex follows early after a previous sinus beat some of the the conducting tissues below may not conduct. A premature atral complex can therefore have different fates (see figure):
- Normally conducted
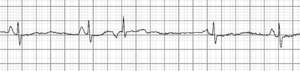
- Conducted with aberrancy. Mostly right bundle branch block aberrancy as the RBBB has a longer refractory period.
- Non-conducted. If the premature beat is very early, the AV node is refractory (cannot conduct) and the beat is not followed by a QRS complex. A non-conducted premature atrial beat is often confused with type II second degree AV block where a normal sinus beat is not followed by a QRS complex.
A premature atrial complex is usually followed by a noncompensatory pause caused by the fact that atrial depolarization enters the sinus node and resets the sinus rhythm.
Premature atrial complexes are common and usually benign. Frequent atrial ectopic beats (>100 / 24hrs) in a population of patients presented to a cardiovascular hospital wass associated with a small chance of 1% of developing atrial fibrillation in the following year [1]
See also:
References
- Suzuki S, Sagara K, Otsuka T, Kano H, Matsuno S, Takai H, Uejima T, Oikawa Y, Koike A, Nagashima K, Kirigaya H, Yajima J, Tanabe H, Sawada H, Aizawa T, and Yamashita T. Usefulness of frequent supraventricular extrasystoles and a high CHADS2 score to predict first-time appearance of atrial fibrillation. Am J Cardiol. 2013 Jun 1;111(11):1602-7. DOI:10.1016/j.amjcard.2013.01.335 |